袁满涓 霍保善
[摘要]目的 探討氧代谢指标中心静脉-动脉二氧化碳分压差与动脉-中心静脉氧含量差比值(Pv-aCO2/Ca-vO2)对脓毒症早期急性肾损伤(AKI)的临床意义。方法 采用前瞻性队列研究方法,选取2019年8月~2020年1月佛山市第二人民医院重症医学科收治的脓毒症行机械通气患者48例,根据复苏24 h后是否发生AKI分为AKI组(n=31)和非AKI组(n=17)。分别收集患者复苏0、12、24 h后的毛细血管再填充时间(CRT)、乳酸(Lac)、Pv-aCO2、Ca-vO2。应用二元Logistic回归模型分析AKI的影响因素,受试者工作特征(ROC)曲线评价指标的敏感度与特异性。结果 入院时AKI组的急性生理学及慢性健康状况评分、序贯器官衰竭评分高于非AKI组,差异有统计学意义(P<0.05),复苏24 h后,AKI组Lac水平高于非AKI组,差异有统计学意义(P<0.05);复苏12、24 h后,AKI组CRT长于非AKI组,差异有统计学意义(P<0.05);复苏0、12、24 h后,AKI组Pv-aCO2/Ca-vO2高于非AKI组,差异有统计学意义(P<0.05)。应用二元Logistic回归分析显示,复苏24 h后Pv-aCO2/Ca-vO2值(β=2.579,OR=13.181,95%CI=1.048~165.708,P=0.046)是脓毒症患者早期AKI发生的独立危险因素。ROC曲线显示,复苏24 h后的Pv-aCO2/Ca-vO2值预测AKI进展的曲线下面积最高,其临界值为1.625,敏感度为83.9%,特异性为76.5%。结论 氧代谢评估对脓毒症患者复苏时早期AKI评估具有重要的临床意义,其中Pv-aCO2/Ca-vO2对AKI病情进展具有较好的预测价值。
[关键词]脓毒性休克;急性肾损伤;微循环与氧代谢评估;毛细血管再填充时间
[中图分类号] R44? ? ? ? ? [文献标识码] A? ? ? ? ? [文章编号] 1674-4721(2020)8(b)-0010-05
[Abstract] Objective To explore the clinical significance of the ratio of the central venous-arterial carbon dioxide partial pressure difference and the arterial-central venous oxygen content difference (Pv-aCO2/Ca-vO2) to early acute renal injury (AKI) in sepsis. Methods This study was a prospective and observative cohort study. A total of 48 patients with sepsis and mechanical ventilation in the intensive care unit of Foshan Second People Hospital were enrolled into this study and their general clinical data grading scores were collected from August, 2019 to January, 2020. According to whether AKI occurred 24 h after resuscitation, they were divided into AKI group (n=31) and non-AKI group (n=17). The capillary refill time (CRT), lactate (Lac), Pv-aCO2 and Ca-vO2 were collected at 0, 12 and 24 h after resuscitation. The potential influencing factors of AKI were analyzed by binary Logistic regression model, and then the risk factors were decided. Receiver operating characteristic curve (ROC) was used to analyze the predictive value of each indexs for AKI diagnostic value at the early stage of sepsis. Results The initial score of acute physiology and chronic health and the initial score of sequential organ failure in AKI group were higher than those in the non-AKI group, the differences were statistic significant(P<0.05). At 24 h after resuscitation, the Lac level in the AKI group was higher than that of the non-AKI group, and the difference was statistically significance(P<0.05); At 12 and 24 h after resuscitation, the CRT of AKI group were longer than those of the non-AKI group, the differences were statistically significant(P<0.05); At 0, 12 and 24 h after resuscitation, the Pv-aCO2/Ca-vO2 of the AKI group were higher than those of non-AKI group, the differences were also statistically significant(P<0.05). The results of binary Logistic regression analysis showed that the value of Pv-aCO2/Ca-vO2 (β=2.579, OR=13.181, 95%CI=1.048-165.708, P=0.046) was an independent risk factor of AKI in early sepsis. ROC curve showed that 24 h after resuscitation, the cutoff value of Pv-aCO2/Ca-vO2 was 1.625, the sensitivity was 83.9% while the specificity was 76.5%. Conclusion Oxygen metabolism assessment has important clinical significance for early AKI assessment during resuscitation. Among them, Pv-aCO2/Ca-vO2 has a good predictive value for the progression of AKI.
[Key words] Septic shock; Acute kidney injury; Microcirculation and oxygen metabolism evaluation; Capillary refill time
目前我国每年至少有290万例成年急性肾损伤(AKI)患者需住院治疗,其中约70万例病死,并且在临床上有严重的漏诊、误诊和治疗不当的情况发生,整体诊疗水平亟待提高[1]。AKI在脓毒症住院患者中具有较高的发生率和病死率,分别为26.9%和11.0%,加强对脓毒症患者AKI的防治对改善患者预后具有重要意义[2]。目前研究认为微循环灌注异常与氧代谢障碍是影响脓毒性休克肾损伤的两个重要因素,因此对脓毒症患者早期微循环和氧代谢的评估是治疗脓毒性AKI的关键[3]。氧输送参数之一的中心静脉-动脉二氧化碳分压差与动脉-中心静脉氧含量差比值(Pv-aCO2/Ca-vO2)是评价无氧代谢的指标,其理论依据是组织消耗的氧减少,所生成的二氧化碳也相应减少,但同时组织无氧代谢时会继发生成二氧化碳,从而出现二氧化碳减少程度小于氧减少程度的情况即表现为Pv-aCO2/Ca-vO2升高[4]。由于该指标可以较好地评估微循环灌注以及细胞无氧代谢情况,目前已经运用到脓毒症休克患者复苏后的病情和预后的评估中[5]。本项目旨在探讨Pv-aCO2/Ca-vO2对脓毒症早期患者AKI发生的诊断价值。
1资料与方法
1.1一般资料
选取2019年8月~2020年1月佛山市第二人民医院重症医学科收治的48例脓毒症患者。纳入标准:①符合2016年美国重症医学会颁布的脓毒症和脓毒性休克管理的国际指南中的相关诊断标准[6];②年龄>18岁且<90岁;③需行有创机械辅助通气。排除标准:①存在通气氧合严重异常者,即吸氧浓度(FiO2)>80%,二氧化碳分压>60 mmHg,呼氣末气道正压>10 cmH2O;②慢性肾功能不全;③患者家属拒绝签署知情同意书;④患者入院24 h内死亡或自动出院。本研究符合医学伦理学标准,经佛山市第二人民医院伦理委员会批准,所有检测和治疗均获得患者家属的知情同意。
1.2方法
收集所有患者的一般临床资料、急性生理学及慢性健康状况评分(APACHEⅡ)、序贯器官衰竭评分(SOFA)。其中APACHEⅡ广泛用于危重症疾病病情分类跟预后预测,分值越高表示病情越重,预后越差。APACHEⅡ包括急性生理评分、年龄评分及慢性健康评分三部分,最后得分为三者之和。理论最高分71分,分值越高病情越严重[7]。SOFA主要内容是评估脏器功能,目的是描述多器官衰竭发生发展并评价发生率,0~48分,分数越高提示预后越差[8]。所有患者均按照脓毒症诊治指南[6]给予相应基础治疗,包括尽早合理应用抗感染药物、机械通气、积极优化血流动力学治疗、镇静镇痛、营养支持等。由于复苏需要,治疗前均留置颈内或锁骨下静脉导管,并经股动脉放置动脉导管,进行有创监测血压。监测内容包括0 h及复苏12 h,24 h的CRT、Lac、Pv-aCO2、Ca-vO2。根据肾脏病预后组织在2012年提出AKI诊断标准[9],将复苏24 h后的患者分为AKI组和非AKI组。
1.3统计学方法
采用SPSS25.0统计学软件进行数据分析。计量资料符合正态分布的用均数±标准差(x±s)表示,非正态分布的计量资料改用中位数(四分位数)[M(Q25,Q75)]表示,符合正态方差齐时采用独立样本t检验,不符合正态或方差不齐的计量资料用Mann-Whitney U检验;计数资料采用χ2检验。应用二元Logistic回归模型分析AKI的影响因素;应用受试者工作特征(ROC)曲线确定诊断临界值。P<0.05为差异有统计学意义。
2结果
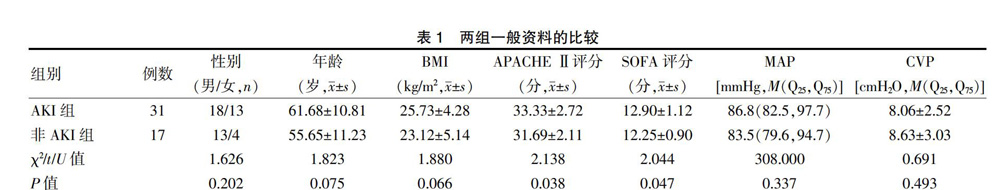
2.1两组一般资料的比较
两组性别、年龄、体重指数(BMI)、动脉压(MAP)、中心静脉压(CVP)比较,差异均无统计学意义(P>0.05)。AKI组的APACHEⅡ、SOFA评分高于非AKI组,差异有统计学意义(P<0.05)(表1)。
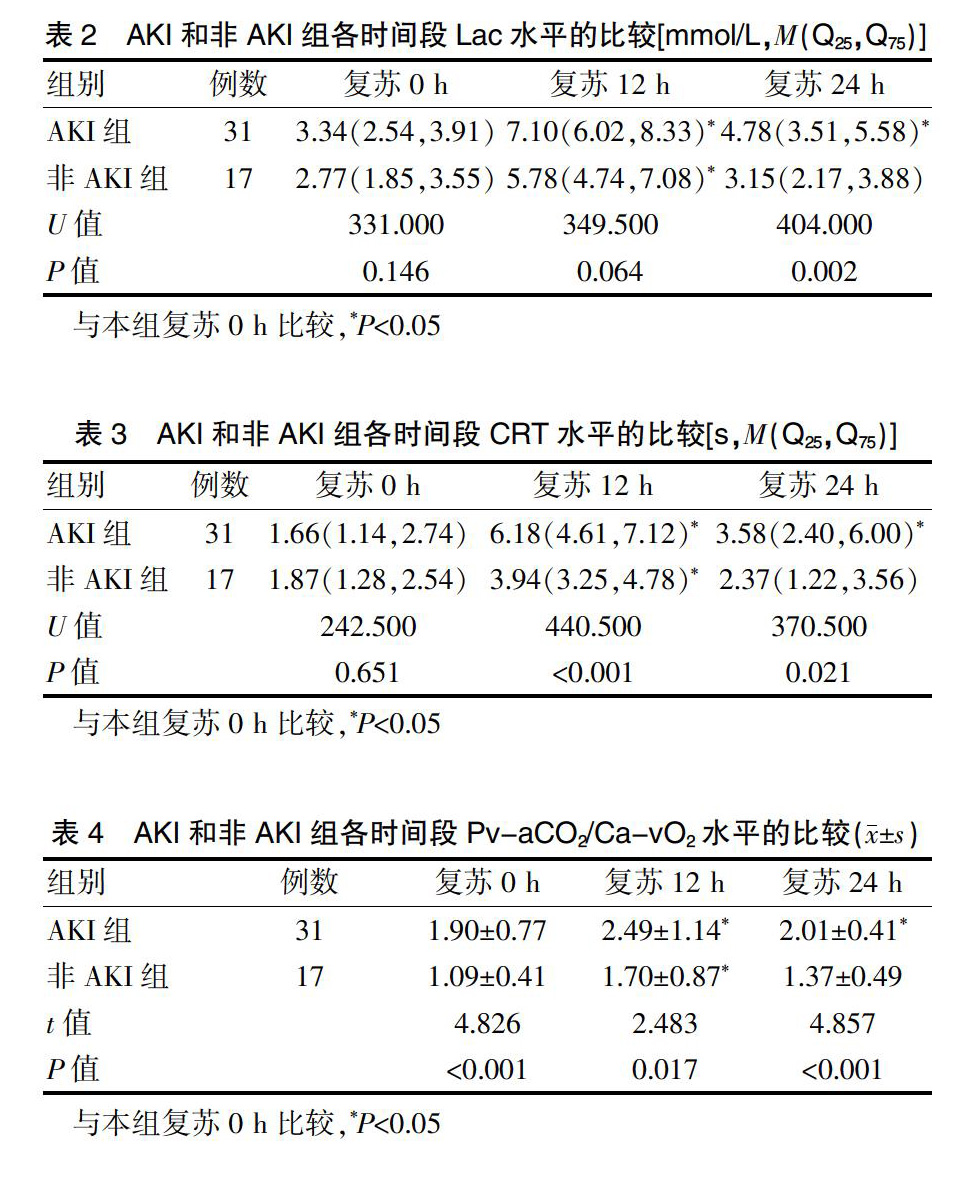
2.2 AKI组和非AKI组各时间段微循环指标的比较
复苏24 h后,AKI组Lac水平高于非AKI组,差异有统计学意义(P<0.05)。复苏12、24 h,AKI组CRT长于非AKI组,差异有统计学意义(P<0.05)。复苏0、12、24 h,AKI组Pv-aCO2/Ca-vO2均高于非AKI组,差异有统计学意义(P<0.05)。组内比较,与复苏0 h比较,AKI组12、24 h两个时间段的Lac、CRT、Pv-aCO2/Ca-vO2微循环指标均升高,差异有统计学意义(P<0.05)。与复苏0 h比较,非AKI组复苏12 h的Lac、CRT、Pv-aCO2/Ca-vO2微循环指标均升高,差异有统计学意义(P<0.05);非AKI组复苏24 h后的Lac、CRT、Pv-aCO2/Ca-vO2微循环指标与复苏0 h比较,差异无统计学意义(P>0.05)(表2~4)。
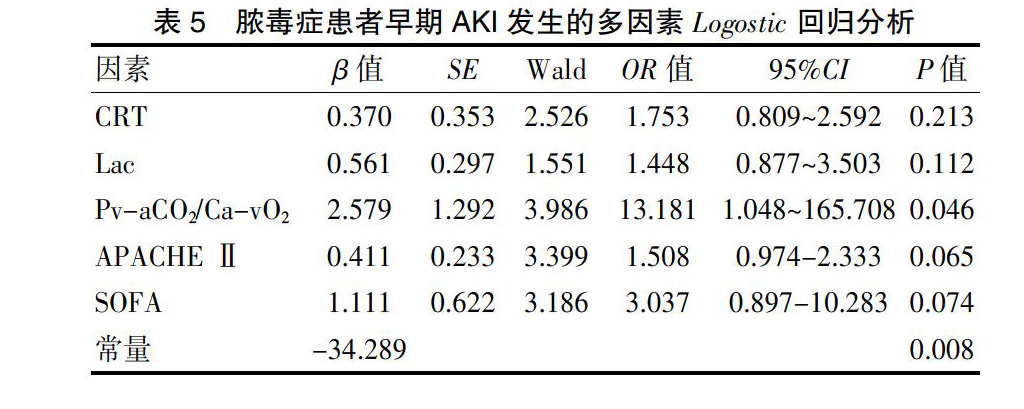
2.3脓毒症患者早期AKI发生的二元Logistic回归分析
以AKI和非AKI为因变量,以CRT、CRT、Lac、Pv-aCO2/Ca-vO2、APACHE Ⅱ、SOFA作为自变量进行二元Logistic回归分析,结果显示Pv-aCO2/Ca-vO2是脓毒症早期AKI发生的独立危险因素(P<0.05)(表5)。
2.4氧代谢标预测AKI的敏感度、特异性
复苏24 h后,CRT、Lac水平、Pv-aCO2/Ca-vO2对AKI的预测价值:根据约登指数,Pv-aCO2/Ca-vO2预测复苏后24 h内AKI进展的临界值为1.625,敏感度为83.9%,特异性为76.5%(表6、图1)。
3討论
AKI是脓毒症患者最常见的并发症,是脓毒症患者死亡风险增加的危险因素。肾血流不足导致的肾小球与肾小管细胞坏死曾被认为是AKI的主要发生机制。近期研究证实,休克患者大循环复苏后,尽管肾血流恢复正常甚至增加,AKI仍会发生[10]。脓毒性休克患者完成早期目标导向治疗并不能降低AKI的发生[11]。肾组织微循环异常与线粒体功能障碍是现在研究证实的AKI发生、发展的重要机制,也是目前脓毒性休克治疗进一步改善预后的难点[12]。休克早期复苏后中心静脉血氧饱和度正常并不能保证组织灌注和细胞氧代谢的恢复,复苏深入到微循环和细胞氧代谢已成为共识[13-14]。在治疗过程种,也发现脓毒症早期患者Lac、CRT等微循指标异常。因此微循环与氧代谢评估成为脓毒性AKI评估的关键。
有学者发现,Pv-aCO2/Ca-vO2可预测快速增加氧输送后氧消耗的反应,Pv-aCO2/Ca-vO2异常升高提示存在无氧代谢,氧输送-氧消耗呈依赖关系,增加氧输送可以相应增加氧消耗[5,15]。作为反映组织缺氧的一项敏感指标,与Lac具有良好的相关性,且能较为准确地预测休克患者液体复苏后氧代谢的变化。Monnet等[5]研究提示,Pv-aCO2/Ca-vO2从理论上作为组织缺氧指标比血浆Lac浓度反应更早、更快、更纯粹。脓毒症性AKI通常发生在入住ICU后24 h内[16-17],在脓毒症休克患者中,约68%的AKI发生在脓毒症诊断后的6 h内[18]。国内现见1例研究,使用氧代谢指标来评估脓毒性休克患者的AKI发生情况[1]。然而入住ICU脓毒症患者不完全出现大循环衰竭,微循环障碍反而多见。早期未发生休克前,预测到AKI的可能性及严重程度更具临床意义。本研究中也观察到,入院时AKI组的APACHEⅡ、SOFA评分高于非AKI组,差异有统计学意义(P<0.05)。复苏24 h后,AKI组Lac水平高于非AKI组,差异有统计学意义(P<0.05);复苏12、24 h,AKI组CRT长于非AKI组,差异有统计学意义(P<0.05);复苏0、12、24 h,AKI组Pv-aCO2/Ca-vO2均高于非AKI组,差异有统计学意义(P<0.05);组内比较,与复苏0 h比较,AKI组12、24 h两个时间段的Lac、CRT、Pv-aCO2/Ca-vO2微循环指标均升高,差异有统计学意义(P<0.05)。与复苏0 h比较,非AKI组复苏12 h的Lac、CRT、Pv-aCO2/Ca-vO2微循环指标均升高,差异有统计学意义(P<0.05);与复苏0 h比较,非AKI组复苏24 h后的Lac、CRT、Pv-aCO2/Ca-vO2微循环指标变化不大,差异无统计学意义(P>0.05)。说明AKI组与非AKI组复苏后12 h与治疗前相比效果明显,经过复苏治疗24 h后,非AKI组指标改善更明显。说明复苏改善了两组患者的病情,非AKI组患者可能因为基础情况良好,微循环指标理想,复苏后效果更为理想。相对于其他脓毒症患者,并发了AKI的患者病情评分明显高于非AKI患者,同时他们的微循环指标也明显降低,说明AKI的发生严重降低了患者生理健康指标,并且加重了他们的多脏器负担。同时通过多因素Logostic回归分析显示,Pv-aCO2/Ca-vO2是脓毒症早期AKI的独立危险因素;根据约登指数,Pv-aCO2/Ca-vO2预测复苏后24 h内AKI进展的临界值为1.625,敏感度为83.9%,特异性为76.5%。可以较好分辨出AKI高风险患者,早期及时予以针对性的治疗。
综上,AKI在脓毒症早期具有较高的发病率,微循环和氧代谢评估对脓毒症早期AKI评估具有重要的临床意义,其中Pv-aCO2/Ca-vO2对AKI病情进展具有较好的预测价值。
[参考文献]
[1]Li Y,Guolan X,Li W,et al.Acute kidney injury in China:a cross-sectional survey[J].Lancet (London,England),2015, 386(10002):1465-1471.
[2]Kaddourah A,Basu RK,Bagshaw SM,et al.Epidemiology of acute kidney injury in critically ill children and young adults[J].N Engl J Med,2017,376(1):11-20.
[3]Seely KA,Holthoff JH,Burns ST,et al.Hemodynamic changes in the kidney in a pediatric rat model of sepsis-induced acute kidney injury[J].Am J Physiol Renal Physiol,2011,301(1):F209-217.
[4]Mesquida J,Saludes P,Gruartmoner G,et al.Central venous-to-arterial carbon dioxide difference combined with arterial-to-venous oxygen content difference is associated with lactate evolution in the hemodynamic resuscitation process in early septic shock[J].Crit Care,2015,19(1):126.
[5]Monnet X,Julien F,Ait-Hamou N,et al.Lactate and venoarterial carbon dioxide difference/arterial-venous oxygen difference ratio,but not central venous oxygen saturation,predict increase in oxygen consumption in fluid responders[J].Crit Care Med,2013,41(6):1412-1420.
[6]Rhodes A,Evans LE,Alhazzani W,et al.Surviving sepsis campaign:international guidelines for management of sepsis and septic shock[J].Crit Care Med,2017,45(3):486-552.
[7]LeGall JR,Loirat P,Alpérovitch A.APACHE II-a severity of disease classification system[J].Crit Care Med,1986,14(8):754-755.
[8]Le Gall JR,Lemeshow S,Saulnier F.A new Simplified Acute Physiology Score(SAPS Ⅱ) based on a European/North American multicenter study[J].JAMA,1993,270(24):2957-2963.
[9]Disease K,Improving Global Outcomes KDIGO.Acute Kidney Injury Work Group:KDIGO clinical practice guideline for acute kidney injury[J].Kidney International Supplement,2012,2(1):1-138.
[10]Gomez H,Ince C,De Backer D,et al.A unified theory of sepsis-induced acute kidney injury:inflammation,microcirculatory dysfunction,bioenergetics,and the tubular cell adaptation to injury[J].Shock,2014,41(1):3-11.
[11]Wasim A,Memon Javed I,Rifat R,et al.Outcome of patients with acute kidney injury in severe sepsis and septic shock treated with early goal-directed therapy in an intensive care unit[J].Saudi J Kidney Dis Transpl,2014,25(3):544-551.
[12]Zuk A,Bonventre JV.Acute kidney injury[J].Annu Rev Med,2016,67:293-307.
[13]ARISE Investigators,ANZICS Clinical Trials Group,Peake SL,et al.Goal-directed resuscitation for patients with early septic shock[J].N Engl J Med,2014,371(16):1496-506.
[14]ProCESS Investigators,Yealy DM,Kellum JA,et al.A randomized trial of protocol-based care for early septic shock[J].N Engl J Med,2014,370(18):1683-1693.
[15]Mallat J,Lemyze M,Meddour M,et al.Ratios of central venous-to-arterial carbon dioxide content or tension to arteriovenous oxygen content are better markers of global anaerobic metabolism than lactate in septic shock patients[J].Ann Intensive Care,2016,6(1):10.
[16]Lima RS,Marques CN,Silva Júnior GB,et al.Comparison between early and delayed acute kidney injury secondary to infectious disease in the intensive care unit[J].Int Urol Nephrol,2008,40(3):731-739.
[17]Bagshaw SM,Lapinsky S,Dial S,et al.Acute kidney injury in septic shock:clinical outcomes and impact of duration of hypotension prior to initiation of antimicrobial therapy[J].Intensive Care Med,2009,35(5):871-881.
[18]Sood Manish M,Anne SL,Julie H,et al.Early reversible acute kidney injury is associated with improved survival in septic shock[J].J Crit Care,2014,29(5):711-717.
(收稿日期:2020-04-07)
- 浅谈职业教育匠心育人的内涵建设
- 基于WebVR的网络教学
- 基于现代学徒制的天线制作课程建设与实践
- 基于高阶累计量的平稳非高斯信号检测
- 航空电子产品通用测试设备架构研究
- 情境学习理论下虚拟数字电路实验平台的设计
- 空调箱中静电过滤器自动排布算法研究
- 计算机硬件虚拟仿真系统的研究与设计
- GPS信息技术在三鑫鞋业有限公司的应用研究
- 现代计算机应用技术对我国企业信息化影响阐述
- 基于ARM的信手拈影智能抽纸盒设计
- 虚拟现实技术在教育领域中的应用
- 基于云计算的智能交通信息采集系统的设计与实现
- 一种改进型硬件红外遥控检测仪的设计与实现
- GSM家用防盗火灾报警系统设计
- 基于Verilog的洗衣机控制电路设计
- 智能窗户感测报警器的开发研究
- 基于STM32的便携式糖化血红蛋白检测系统
- 小尺寸团簇电子的分裂能级统计特征
- 基于NB—IoT的电焊机集群监控系统的设计
- CITRIX桌面虚拟化技术及其优势分析
- 基于HOLT芯片的1553B总线通信接口的设计
- 基于Verilog语言的数字跑表电路设计
- 基于Verilog语言的4位二进制可逆计数器的设计
- 基于FPGA的环形计数器设计
- congregates
- congregating
- congregation
- congregational
- congregationer
- congregationist
- congregations
- congregative
- congregativeness
- congregativenesses
- congregator
- congregators
- congress
- congressed
- congresses
- congressing
- congression
- congressional
- congressionalists
- congressionally
- congressist
- congressman
- congressman/congresswoman
- congressman / congresswoman
- congressmen
- 佥事
- 佥人
- 佥佐
- 佥允
- 佥同
- 佥名
- 佥士
- 佥壬
- 佥宪
- 佥票
- 佥都御史
- 佥院
- 佧
- 佧佤
- 佧佤族
- 佩
- 佩兰
- 佩兰客
- 佩兰应梦
- 佩凤
- 佩刀
- 佩刀剑上的装饰
- 佩刀的来历
- 佩刀的玉饰
- 佩刀鞘上近口处的饰物