徐爱静 孔德亮 李双喜


[摘要] 目的 分析特利加压素治疗肝硬化腹水相关性急性肾损伤(AKI)Ⅰ期患者的效果及复发情况。 方法 收集2014年1月—2018年2月于长海医院住院治疗的123例肝硬化腹水AKI Ⅰ期患者的临床资料,采用随机数字表法分为对照组(n = 56)和观察组(n = 67)。对照组给予常规治疗,观察组在此基础上加用特利加压素。并对所有患者随访6个月,评估两组临床疗效,比较两组治疗前及随访结束后总胆红素(TBil)、丙氨酸氨基转移酶(ALT)、白蛋白、血肌酐(Scr)、血钠、国际标准化比值(INR)、终末期肝病模型(MELD)评分、终末期肝病模型-钠(MELD-Na)评分和估算的肾小球滤过率(eGFR)水平,比较两组复发率。 结果 两组治疗前的TBil、ALT、白蛋白、Scr、血钠、血尿素氮(BUN)、INR、MELD评分、MELD-Na评分比较,差异无统计学意义(P > 0.05),但观察组治疗前的eGFR低于对照组(P < 0.05)。两组随访结束后的TBil、ALT、Scr、INR均低于治疗前,白蛋白、MELD评分、MELD-Na评分和eGFR均高于治疗前(P < 0.05),且观察组随访结束后的TBil、Scr、BUN均低于對照组,白蛋白、MELD-Na评分和eGFR均高于对照组(P < 0.05)。观察组住院天数明显短于对照组,治疗应答率明显高于对照组,差异有统计学意义(P < 0.05)。随访1、3、6个月两组的复发率及总复发率比较,差异无统计学意义(P > 0.05)。结论 特利加压素治疗肝硬化腹水AKI Ⅰ期患者能有效降低Scr、BUN,提高白蛋白、eGFR,改善患者肾功能,缩短患者住院时间,但对降低其复发率无显著效果。
[关键词] 特利加压素;肝硬化;急性肾损伤;疗效
[中图分类号] R692? ? ? ? ? [文献标识码] A? ? ? ? ? [文章编号] 1673-7210(2020)10(b)-0111-04
[Abstract] Objective To analyze the efficacy and recurrence rate of Terlipressin in the treatment of ascites-related acute renal injury (AKI) stage Ⅰ patients with cirrhosis. Methods Clinical data of 123 patients with AKI stage Ⅰ cirrhosis ascites treated in Changhai Hospital from January 2014 to February 2018 were collected and randomly divided into control group (n = 56) and observation group (n = 67) according to random number table method. Control group was given conventional treatment, and observation group was given Terlipressin on this basis. All patients were followed up for six months. Clinical efficacy of two groups was evaluated. The levels of total bilirubin (TBil), alanine aminotransferase (ALT), albumin, serum creatinine (Scr), serum sodium, international normalized ratio (INR), end-stage liver disease (MELD) score, MELD-Na score and estimated glomerular filtration rate (eGFR) were compared between two groups before treatment and after follow-up. The recurrence rate was compared between two groups. Results There were no significant differences in TBil, ALT, albumin, Scr, serum sodium, blood urea nitrogon (BUN), INR, MELD-Na score between two groups before treatment (P > 0.05). But eGFR of observation group was lower than that of control group before treatment (P < 0.05). TBil, ALT, Scr and INR of two groups after follow-up were lower than those before treatment, while albumin, MELD score, MELD-Na score and EGFR were higher than those before treatment (P < 0.05). TBil, Scr and BUN of observation group were lower than those of control group after follow-up, while albumin, MELD-Na score and eGFR of observation group were higher than those of control group (P < 0.05). The length of stay in observation group was significantly shorter than that in control group, and treatment response rate was significantly higher than that in control group (P < 0.05). There were no significant differences in recurrence rate and total recurrence rate between two groups after one, three and six months of follow-up (P > 0.05). Conclusion Terlipressin in the treatment of cirrhotic ascites AKI stage Ⅰ patients can effectively reduce Scr, BUN, albumin and eGFR, improve renal function, shorten the length of hospital stay, but has no significant effect on reducing the recurrence rate of AKI.
[Key words] Terlipressin; Cirrhosis; Acute kidney injury; Efficacy
急性肾损伤(AKI)作为肝硬化的常见并发症,具有较高的发生率,且与不良预后存在显著正相关[1-2]。研究表明,肝硬化相关的AKI常见病因表型为肾前无氮血症(PRA)、急性肾小管坏死(ATN)和肝肾综合征(HRS)[3]。目前已有的诊疗手段对肝硬化腹水AKI收效甚微[4-5],已成为肝病治疗中的棘手问题[6]。肝硬化患者AKI最新管理系统认为,对HRS-AKI患者,应早期应用血管收缩剂,如特利加压素、去甲肾上腺素等[7]。研究表明,约40%的HRS患者对血管收缩和白蛋白的联合治疗有效[8]。特利加压素是一种新型人工合成的血管加压素类似物,具有明确的缩血管功效,在临床上广泛应用于HRS、肝硬化腹水等治疗[9-10]。本研究对特利加压素治疗肝硬化腹水AKI Ⅰ期患者的效果、预后及复发率进行临床研究,为其临床应用提供更多依据。
1 资料与方法
1.1 一般资料
选取2014年1月—2018年2月于长海医院住院治疗的肝硬化腹水相关性AKI Ⅰ期患者123例,其中观察组67例,男51例,女16例;年龄50~65岁,平均(57.14±10.71)岁。对照组56例,男45例,女11例;年龄50~64岁,平均(56.37±9.69)岁。两组患者一般资料比较,差异无统计学意义(P > 0.05),具有可比性。
1.2 纳入及排除标准
纳入标准:①符合2015年国际腹水协会(ICA)HRS-AKI Ⅰ期临床诊断且诊断明确[11];②临床资料完整;③首次诊断、初始治疗者。排除标准:①入组前应用肾毒性药物及严重结构性肾损伤患者;②对研究存在异议患者;③严重基础疾病或并发症患者;④严重心脑血管疾病患者;⑤恶病质患者;⑥仅进行过1次血肌酐(Scr)水平检测的患者。
1.3 诊断标准
根据ICA提出的肝硬化患者AKI新诊断标准:AKI分期Ⅰ期:Scr升高≥ 26.5 mmol/L,或高于基线水平1.5~2.0倍[12]。
1.4 治疗方案
对照组患者给予原发病治疗和一般支持治疗,包括保肝、利尿、抗感染、抗病毒、营养支持等;观察组在上述治疗基础上给予特利加压素(深圳翰宇药业股份有限公司,国药准字H20093804,1 mg)3~4 mg/d。1 mg加入0.9%氯化钠注射液100 mL静脉缓慢滴注(维持1 h),每6~8小时1次,疗程均为7 d。
1.5 观察指标
观察两组治疗前及随访结束后总胆红素(TBil)、丙氨酸氨基转移酶(ALT)、白蛋白、Scr、血尿素氮(BUN)、血钠、国际标准化比值(INR)、终末期肝病模型(MELD)评分、终末期肝病模型-钠(MELD-Na)评分和估算的肾小球滤过率(eGFR)水平。观察两组患者疾病预后,随访6个月,观察AKI的复发率。MELD计算公式:MELD分值=3.8×ln(TBiL水平)+11.2×ln(INR)+9.6×ln(Scr水平)+6.4×病因(病因:胆汁性或酒精性为0,其为1)。MELD-Na分值=MELD+1.59×(135-Na)。eGFR公式:eGFR(mL/min·1.73m2)=1.86×Scr-1.154×年龄-0.203×0.742女性。
1.6 临床效果判定
临床疗效包括住院天数和AKI治疗应答率,定义[5],AKI治疗无应答:AKI无恢复;AKI治疗部分应答:AKI Ⅰ分期下降及Scr降低至基线值≥26.5 μmol/L;AKI治疗完全应答:Scr降低至基线值26.5 μmol/L以内。治疗应答率=(部分应答+完全应答)/总例数×100%。
1.7 统计学方法
采用SPSS19.0统计学软件处理数据。符合正态分布的计量资料用均数±标准差(x±s)表示,组间比较采用独立样本t检验,组内比较采用配对t检验;不符合正态分布的计量资料用中位数(四分位数)[M(P25,P75)]表示,采用秩和检验。计数资料用[例(%)]表示,组间比较采用χ2检验。以P < 0.05为差异有统计学意义。
2 结果
2.1 两组患者治疗前后相关观察指标水平比较
两组治疗前的TBil、ALT、白蛋白、Scr、血钠、BUN、INR、MELD评分、MELD-Na评分比较,差异无统计学意义(P > 0.05),但观察组治疗前的eGFR低于对照组(P < 0.05);两组随访结束后的TBil、ALT、Scr、INR均低于治疗前(P < 0.05),白蛋白、MELD评分、MELD-Na评分和eGFR均高于治疗前(P < 0.05),且观察组随访结束后的TBil、Scr、BUN均低于对照组(P < 0.05),白蛋白、MELD-Na评分和eGFR均高于对照组(P < 0.05)。见表1。
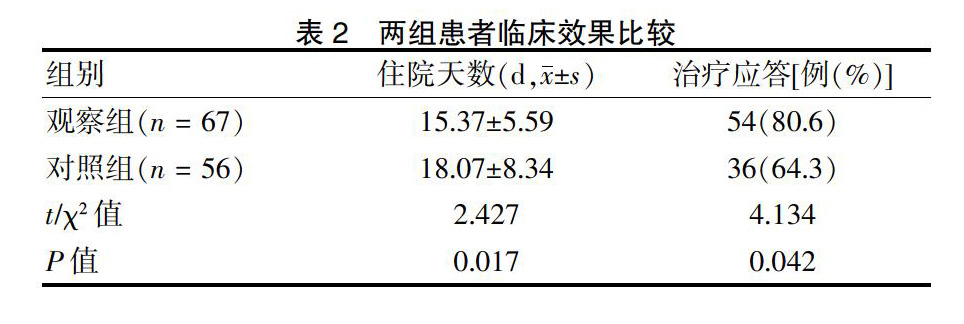
2.2 两组患者临床效果比较
2.3 两组患者随访复发率比较
3 讨论
AKI主要表现为eGFR急剧下降,Scr和BUN迅速升高和伴水钠潴留,这些症状是重癥患者预后不良的征兆和死亡的独立预测参数[13]。HRS是AKI较为常见且危害较为严重的一种,未经治疗的Ⅰ型HRS生存预后极差,多数不足3个月[6,14]。相反,Ⅱ型HRS患者中位生存期6个月左右[15-16]。对此,本研究探讨特利加压素对肝硬化腹水相关性AKI Ⅰ期患者的疗效,预后及对AKI复发的影响,欲为后期此类患者的临床治疗提供新的思路与方法。
与其他原因引起的肾前性AKI不同,HRS是肝硬化患者严重的功能性肾损伤。临床研究结果表明,在约25%的患者中,使用血管收缩剂和白蛋白治疗肾功能明显改善[17]。本研究结果显示,特利加压素治疗肝硬化腹水AKI Ⅰ期患者能有效降低Scr、BUN水平,提高eGFR水平,改善患者肾功能。临床实践表明,血管收缩剂的使用多有明显不良反应,而特利加压素相对较轻,最为明显的是患者应用后无明显的缺血反应,且临床效果明确[18]。有研究显示,HRS患者应用特利加压素治疗后对Scr水平、生存率以及逆转率均有积极的作用[19]。本研究结果显示,观察组患者住院天数明显短于对照组。另外,研究发现,短期特利加压素治疗对抑制HRS-AKI的复发具有积极作用,但中长期预防效果不明显,与有关研究[20]结果基本一致,提示血管收缩剂对降低HRS的复发率效果不明显。
综上所述,临床对于HRS-AKI Ⅰ期患者,应早期应用血管收缩剂-特利加压素治疗,以取得更佳的预后效果。
[参考文献]
[1]? Hamdy HS,El-Ray A,Salaheldin M,et al. Urinary neutrophil gelatinase-associated lipocalin in cirrhotic patients with acute kidney injury [J]. Ann Hepatol,2018,17(4):624-630.
[2]? Belcher JM,Sanyal AJ,Peixoto AJ,et al. Kidney biomarkers and differential diagnosis of patients with cirrhosis and acute kidney injury [J]. Hepatology,2014,60(2):622-632.
[3]? Xiong J,Pu L,Xiong H,et al. Evaluation of the criteria of hepatorenal syndrome type of acute kidney injury in patients with cirrhosis admitted to ICU [J]. Scand J Gastroenterol,2018,53:1590-1596.
[4]? Jaques DA,Spahr L,Berra G,et al. Biomarkers for acute kidney injury in decompensated cirrhosis:a prospective study [J]. Nephrology,2019,24(2):170-180.
[5]? Patil V,Jain M,Venkataraman J. Paracentesis-induced acute kidney injury in decompensated cirrhosis-prevalence and predictors [J]. Clin Exp Hepatol,2019,5(1):55-59.
[6]? Chancharoenthana W,Leelahavanichkul A. Acute kidney injury spectrum in patients with chronic liver disease:where do we stand? [J]. World J Gastroenterol,2019,25(28):3684-3703.
[7]? Wong F. Treatment to improve acute kidney injury in cirrhosis [J]. Curr Treat Options Gastroenterol,2015,13(2):235-248.
[8]? 邢枫,李爽,张建军,等.特利加压素对顽固性肝硬化腹水的治疗作用与效应特点观察[J].中华肝脏病杂志,2019, 27(12):982-988.
[9]? Kam PC,Williams S,Yoong FF. Vasopressin and terlipressin:pharmacology and its clinical relevance [J]. Anaesthesia,2004,59(10):993-1001.
[10]? 程丹颖,万钢,欧蔚妮,等.特利加压素联合白蛋白治疗肝硬化急性肾损伤的临床疗效观察[J].中华肝脏病杂志,2019,27(9):704-707.
[11]? Angeli P,Ginès P,Wong F,et al. Diagnosis and management of acute kidney injury in patients with cirrhosis:revised consensus recommendations of the International Club of Ascites [J]. J Hepatol,2015,62(4):968-974.
[12]? Paolo A,Pere G,Florence W,et al. Diagnosis and management of acute kidney injury in patients with cirrhosis:revised consensus recommendations of the International Club of Ascitesq [J]. Gut,2015,64(4):531-537.
[13]? Bongers C,Alsady M,Nijenhuis T,et al. Impact of acute versus prolonged exercise and dehydration on kidney function and injury [J]. Physiol Rep,2018,6(11):e13734.
[14]? Lei L,Li L,Zhang H. Advances in the diagnosis and treatment of acute kidney injury in cirrhosis patients [J]. Biomed Res Int,2017,2017:8523649.
[15]? Angeli P,Garcia-Tsao G,Nadim MK,et al. News in pathophysiology,definition and classification of hepatorenal syndrome:a step beyond the International Club of Ascites (ICA) consensus document [J]. J Hepatol,2019, 71(4):811-822.
[16]? Park SK,Ryoo JH,Oh CM,et al. The risk of type 2 diabetes mellitus according to 2-hour plasma glucose level:the Korean Genome and Epidemiology Study(KoGES) [J]. Diabetes Res Clin Pract,2018,146:130-137.
[17]? Boyer TD,Sanyal AJ,Wong F,et al. Terlipressin plus albumin is more effective than albumin alone in improving renal function in patients with cirrhosis and hepatorenal syndrome type 1 [J]. Gastroenterology,2016,150(7):1579-1589.
[18]? Demiselle J,Fage N,Radermacher P,et al. Vasopressin and its analogues in shock states:a review [J]. Ann Intensive Care,2020,10(1):9.
[19]? Wang H,Liu A,Bo W,et al. Terlipressin in the treatment of hepatorenal syndrome:a systematic review and meta-analysis [J]. Medicine(Baltimore),2018,97(16):e0431.
[20]? 熊號峰,刘景院.肝肾综合征研究进展[J].中国肝脏病杂志:电子版,2017,9(1):1-6.
(收稿日期:2020-02-27)
- 天津市跨境电子商务发展的问题及对策
- 基于Android平台的淘医宝系统的设计与实现
- 基于关系型数据库的中医胃腕痛病诊疗数据库的构建及研究性探索
- 基于SQLserver2014+ASP.NET的关联规则分析在产品销售中的应用研究
- 可信计算下数据安全存储研究
- 学生档案管理系统安全问题研究
- 基于SpatialHadoop云平台下空间数据存储研究
- 数据库索引技术概述
- SQL在VisualFoxpro数据库中的应用
- 大数据时代计算机信息处理技术分析
- 数据库技术在山西气象业务中的应用
- SQL注入攻击及其防范技术研究
- 数字媒体技术对动画设计的影响研究
- 基于Internet的多媒体教学系统设计
- 新媒体环境下新闻类微信公众号编辑的实用思维
- 智能车库车辆引导系统的设计
- 基于机器学习的软件缺陷识别的必要性
- 基于树莓派和PICameraV2的动态目标检测
- 深度学习下的推荐系统研究
- 基于视觉和语义的图像检索技术研究
- 基于KNN算法的手写数字识别
- 四足机器人步态位姿及高效行进步态优化研究
- 射频识别RFID技术在智能停车场管理系统中的应用
- 停车场智能停车引导系统
- 一个基于超像素的图像分割算法
- nonpunctually
- nonpunctualness
- nonpunctualnesses
- nonpunctuating
- nonpunctuation
- nonpunctuations
- nonpuncturable
- nonpungencies
- nonpungency
- non-pungent
- nonpungent
- nonpungently
- nonpunishable
- nonpunishing
- nonpunishment
- nonpunishments
- non-punitive
- nonpunitive
- nonpunitory
- nonpurchase
- non-purchase
- nonpurchaser
- nonpurchasers
- nonpurchases
- nonpurification
- 套盒
- 套着烂
- 套着脖子的狗不能打猎
- 套磁
- 套礼
- 套票
- 套种
- 套笼头
- 套索
- 套红
- 套级
- 套色
- 套菜
- 套袋碗
- 套袖
- 套装
- 套裙
- 套裤
- 套词
- 套话
- 套语
- 套购
- 套路
- 套车
- 套车埋老鼠——小题大做