超声引导腹横肌平面阻滞联合纳布啡在日间妇科腹腔镜手术中的应用效果
易艳萍 王琼 程秋菊
[摘要]目的 研究超聲引导腹横肌平面(TAP)阻滞联合纳布啡在日间妇科腹腔镜手术中的应用效果。方法 选取2017年8月~2018年1月经我院妇科门诊与麻醉疼痛门诊筛选进行日间妇科腹腔镜手术的113例患者作为研究对象,将其随机分为实验组(T组,n=45)与对照组(N组,n=68)。T组患者术前进行TAP神经阻滞,N组患者未进行。两组患者均采用相同的全麻诱导、术中麻醉维持与机械通气模式,在手术结束前10 min静脉注射纳布啡0.2 mg/kg,在复苏室如患者视觉模拟量表(VAS)评分>3分时再次静脉注射纳布啡0.15 mg/kg。记录两组患者术前、切皮与拔管时的平均动脉压(MAP)与心率(HR),并观察两组患者的术中瑞芬太尼用量、术毕拔管时间、复苏室再次注射纳布啡比例、在复苏室与术后8 h VAS评分、术后进食时间、术后下床活动时间、恶心呕吐发生率及术后麻醉相关并发症发生情况。结果 N组患者切皮、拔管时的MAP、HR均高于术前,差异有统计学意义(P<0.05);T组患者切皮、拔管时的MAP、HR均低于N组,差异有统计学意义(P<0.05)。T组患者的术中使用瑞芬术尼量少于N组,术毕拔管时间短于N组,差异有统计学意义(P<0.05)。T组患者的复苏室再次注射纳布啡占比为8.89%,明显低于N组的35.29%,差异有统计学意义(P<0.05);两组患者的术后恶心呕吐发生率比较,差异无统计学意义(P>0.05)。T组患者复苏室、术后8 h的VAS评分均低于N组,差异有统计学意义(P<0.05);T组患者的进食时间及下床活动时间均早于N组,差异有统计学意义(P<0.05)。两组患者术后12 h内均未应用阿片类药物镇痛,术后均无呼吸抑制情况发生。结论 术前TAP阻滞能减少术中阿片类药物的使用,纳布啡对患者的内脏疼痛效果佳,两者合用可提高患者的镇痛效果和舒适度,促进日间妇科腹腔镜手术患者的早期康复。
[关键词]腹横肌平面阻滞;纳布啡;镇痛;日间妇科腹腔镜手术;视觉模拟量表
[中图分类号] R614.4? ? ? ? ? [文献标识码] A? ? ? ? ? [文章编号] 1674-4721(2019)8(c)-0111-05
[Abstract] Objective To investigate the application effect of ultrasound-guided transverses abdominis plane (TAP) block combined with Nalbuphine in daytime gynecological laparoscopic surgery. Methods From August 2017 to January 2018, 113 patients who underwent daytime gynecological laparoscopic surgery after screening in gynecological clinics and anesthesia pain clinics of our hospital were selected as the study subjects and they were randomly divided into the experimental group (group T, n=45) and the control group (group N, n=68). Patients in group T underwent TAP nerve block before surgery, and patients in group N did not. The same general anesthesia induction, intraoperative anesthesia maintenance and mechanical ventilation mode were used in both groups. The 0.2 mg/kg Nalbuphine was injected into the vein 10 minutes before the end of surgery in both groups. In the resuscitation room, if the patients′ visual analogue scale (VAS) score >3 points, the Nalbuphine was again intravenously administered at 0.15 mg/kg. The mean arterial pressure (MAP) and heart rate (HR) were recorded before surgery, at incision and extubation in both groups. The intraoperative dose of Remifentanil, the time of extubation, the proportion of re-injection of Nalbuphine in the resuscitation room, the VAS scores in the resuscitation room and 8 h after surgery, the postoperative eating time, the time of postoperative outpatient activity, the incidence rate of nausea and vomiting and the incidence of anesthesia-related complications after surgery were observed in the two groups. Results The MAP and HR of the group N at incision and extubation were higher than those before the surgery, and the differences were statistically significant (P<0.05). The MAP and HR of the patients in the group T at incision and extubation were lower than those in the group N, and the differences were statistically significant (P<0.05). The intraoperative dose of Remifentanil in the group T was less than that in the group N, the time of extubation was shorter than that in the group N, and the differences were statistically significant (P<0.05). The proportion of re-injection of Nalbuphine in the resuscitation room of patients in group T was 8.89%, which was significantly lower than that in group N (35.29%), and the difference was statistically significant (P<0.05). There was no significant difference in the incidence rate of postoperative nausea and vomiting between the two groups (P>0.05). The VAS scores of the resuscitation room and 8 hours after surgery in the group T were lower than those in the group N, and the differences were statistically significant (P<0.05). The eating time and the time of postoperative outpatient activity in the group T were earlier than those in the group N, and the differences were statistically significant (P<0.05). Opioid analgesia was not used in the two groups within 12 hours after surgery, and no respiratory depression occurred after surgery. Conclusion Preoperative TAP block can reduce the use of intraoperative opioids, and Nalbuphine has a good effect on the visceral pain of patients. The combination can improve the analgesic effect and comfort of patients, and promote the early rehabilitation of patients undergoing daytime gynecological laparoscopic surgery.
[Key words] Transversus abdominis plane block; Nalbuphine; Analgesia; Daytime gynecolcogical laparoscopic surgery; Visual analogue scale
日间妇科腹腔镜手术为微创手术,具有手术时间短、创伤较小、疼痛程度较轻、恢复快、住院时间更短等优点,但日间手术成功实施的必要条件是充分的术中与术后镇痛。疼痛主要来源于躯体和内脏疼痛两部分,传统的阿片类药物自控镇痛和椎管内镇痛技术已不再适用于日间疼痛管理。为了患者更充分的镇痛,并减少阿片类药物用量及副作用,更高质量的尽早出院,本研究采用术前腹横肌平面(transverses abdominis plane,TAP)阻滞联合术后静注纳布啡的镇痛技术,现报道如下。
1资料与方法
1.1一般资料
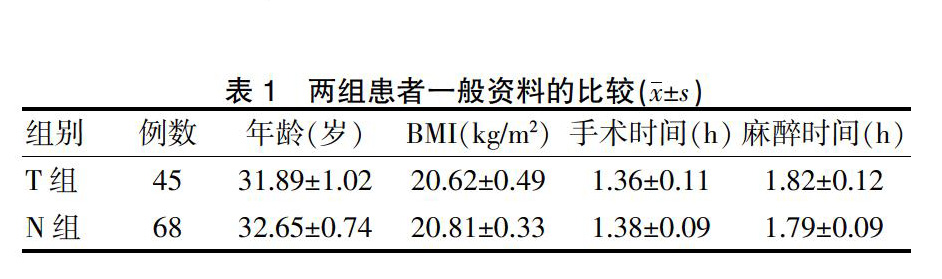
选取2017年8月~2018年1月经我院妇科门诊与麻醉疼痛门诊筛选进行日间妇科腹腔镜手术的113例患者作为研究对象,将其随机分为实验组(T组,n=45)与对照组(N组,n=68)。纳入标准:ASA分级Ⅰ~Ⅱ级;年龄20~60岁;术前患者均签署麻醉知情同意书。排除标准:心血管疾病、肝、肾功能异常、凝血功能异常、罗哌卡因过敏史、神经系统疾病等;神经肌肉功能障碍或术前使用对神经肌肉功能有影响的药物。两组患者的年龄、体重指数(BMI)、手术时间、麻醉时间等一般资料比较,差异无统计学意义(P>0.05)(表1),具有可比性。本研究经医院医学伦理委员会审核批准。
表1? ?两组患者一般资料的比较(x±s)
1.2麻醉方法
入室后常规开放外周静脉通路,监测心电图、心率(HR)、无创血压(如手术时间>1 h或出血多等原因行有创测压)、脉搏氧饱和度、呼气末二氧化碳分压(PETCO2)、脑电双频指数(BIS),静脉输注乳酸钠林格氏液10 ml/(kg·h),术前静脉注射帕络诺司琼(上海华源药业,国药准字 H20080748)0.25 mg;麻醉诱导:面罩去氮给氧,静脉注射盐酸戊乙奎醚注射液(成都力思特制药股份有限公司,国药准字 H20020606)0.3 mg、丙泊酚(Frdsenius Kabi Deutschland GmbH D-61345 Bad Homburg V.d.H.,国药准字 H20160360)2~3 mg/kg、舒芬太尼(宜昌人福药业,国药准字 H200554171)0.3 μg/kg、顺式阿曲库铵(江苏恒瑞医药股份有限公司,国药准字 H20060869)0.3 mg/kg后,行气管插管;机械通气设置通气参数为潮气量8~10 ml/kg,通气频率为12 次/min,吸呼比为1:2,吸入浓度(FiO2)50%氧流量为2 L/min。T组患者在全麻后术前行超声引导下行双侧TAP阻滞,每侧阻滞药物为0.25%罗哌卡因(AstraZeneca AB,国药准字 H20140763)20 ml,N组患者不行TAP阻滞。麻醉维持以6%地氟烷(Baxter Healthcare Puerto Rico,国药准字 H20140187)吸入,静脉泵注丙泊酚6~8 mg/(kg·h)和瑞芬太尼0.15 μg/(kg·min)。全麻过程中采用北京华翔多功能监护仪监测BIS,维持BIS值在45~55,术中根据平均动脉压(MBP)和HR波动幅度不超过基础值的20%及BIS值变化进行调整地氟醚的吸入浓度和瑞芬太尼的输注量。术中维持尿量>1 ml/(kg·h),机械通气将PETCO2维持在35~45 mmHg。在手术结束前10 min静脉注射纳布啡(宜昌人福药业,81J09021)0.2 mg/kg,在复苏室当患者视觉模拟量表(VAS)评分>3分时,静脉注射纳布啡0.15 mg/kg。术毕停用地氟烷。待自主呼吸潮气量达6 ml/kg后拔除气管导管,生命体征平稳送回麻醉恢复室观察30 min,清醒后送回日间病房。达至离院标准后,患者必须在一位有责任能力的成人陪同下出院,并告知患者出院后的有关注意事项。
1.3观察指标及评价标准
记录两组患者术前、切皮与拔管时的MAP与HR,并观察术中瑞芬太尼用量、术毕拔管时间、复苏室再次注射纳布啡的比例、在复苏室与术后8 h VAS评分、术后进食时间、术后下床活动时间、恶心呕吐发生率及术后麻醉相关并发症发生情况。VAS评分:0分表示无痛;>0~3分表示有轻微的疼痛,能忍受;>3~6分表示疼痛并影响睡眠,尚能忍受;>6~10分表示有强烈的疼痛,不能忍受,影响食欲与睡眠。麻醉相关并发症发生情况包括阿片类药物镇痛使用、术后呼吸抑制。日間手术离院标准[1](postanesthesia discharge score,PADS),根据生命体征、活动状态、疼痛、恶心呕吐和手术出血情况,每项2分,满分为10分,PADS评分≥9分则达到离院标准。
1.4统计学方法
采用SPSS 13.0统计学软件进行数据分析,计量资料用均数±标准差(x±s)表示,两组间比较采用t检验;计数资料采用率表示,组间比较采用χ2检验,以P<0.05为差异有统计学意义。
2结果
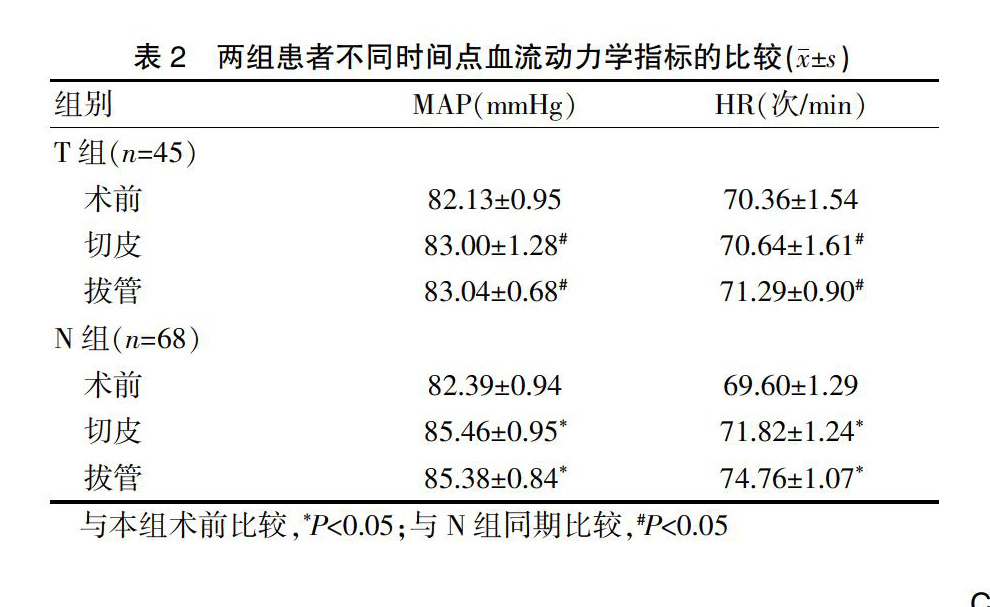
2.1两组患者不同时间点血流动力学指标的比较
两组患者术前的MAP、HR比较,差异无统计学意义(P>0.05);N组患者切皮、拔管时的MAP、HR均高于术前,差异有统计学意义(P<0.05);T组患者切皮、拔管时的MAP、HR与术前比较,差异无统计学意义(P>0.05);T组患者切皮、拔管时的MAP、HR均低于N组,差异有统计学意义(P<0.05)(表2)。
2.2两组患者术中使用瑞芬太尼量、术毕拔管时间的比较
2.3兩组患者复苏室注射纳布啡占比、术后恶心呕吐发生率的比较
2.4两组患者不同时间点VAS评分、饮水时间及下床活动时间的比较
2.5两组患者麻醉相关并发症的发生情况
两组患者术后12 h内均未应用阿片类药物镇痛,术后均无呼吸抑制情况发生。两组患者均在入院24 h内达到日间手术离院标准并离院。出院后5~7 d能恢复日常的生活与工作,未见麻醉相关并发症发生。
3讨论
疼痛作为应激及炎症反应的始发因素,延缓多器官的功能恢复,而良好的镇痛在快速康复外科中占重要地位,有助于预防循环和呼吸系统并发症的发生,改善术后转归,尽早回归日常生活。
本研究结果显示,T组患者使用瑞芬太尼的总剂量少于N组,切皮时的血流动力学更稳定(P<0.05),提示手术开始前实施TAP阻滞,能有效阻断交感神经兴奋的传入,起到超前镇痛的效果,降低痛觉过敏发生率,降低机体的应激反应,手术切皮时不需增加阿片类药物的用量。两组患者在手术结束前10 min静脉注射纳布啡0.2 mg/kg,T组患者比N组更早停用全麻用药,比N组更早拔除气管导管,T组患者拔管时的血流动力学更稳定。超前镇痛是伤害性刺激作用于机体之前给予的镇痛干预,阻断外周的不良刺激传人中枢,同时可抑制术后剧烈疼痛。TAP阻滞是在腋中线处的腹内斜肌与腹横肌之间的神经筋膜层注射局麻药,阻断胸7~腰1脊神经发出外侧皮支中的前皮支,对前腹皮肤、肌肉及壁层腹膜的镇痛效果较好[2],阻断了手术时伤害刺激的传导,避免了中枢神经敏化的形成,有助于预防痛觉过敏及感觉异常的发生[3-4]。现已在下腹部手术的术后镇痛中广泛应用[5]。周春莲等[6]研究发现,术前行超声引导下TAP阻滞比术后进行TAP阻滞能为妇科腹腔镜手术患者提供更好的术后镇痛。而Ali等[7]证实TAP阻滞的镇痛效果可作为腹壁手术硬膜外麻醉的一个有效替代。Ma等[8]研究发现,TAP阻滞能缓解24 h内术后疼痛,至第1次止痛要求时间延迟,减少消耗和延缓阿片类药物的需求,优于伤口局麻醉药浸润和硬膜外阻滞,与国内牟俊英等[9]研究结果相似。
日间病房的医务人员鼓励患者尽早进食与下床活动,本研究结果显示,T组患者有更早的进食、下床活动的意愿及行动(P<0.05),两组患者均在入院24 h内离院,提示TAP阻滞可减弱术后应激和免疫抑制,促进术后肠蠕动恢复,有助于早期进行肠内营养,促进肠功能恢复。多项研究[10-13]已证实,TAP阻滞能减轻妇科腹腔镜手术患者的疼痛,减少并延迟对阿片类药物的需求,降低恶心呕吐发生率,加快患者术后康复,提高患者满意度。
T组患者的术后VAS评分低于N组,N组中更多的患者使用了纳布啡(P<0.05),提示T组的镇痛效果比N组好。腹腔镜下妇科手术对腹膜牵挂、盆腔脏器的刺激均会使患者术后疼痛或不适,采用超声引导下TAP神经阻滞不能阻滞脏层腹膜及内脏神经交感与副交感神经,所以对内脏疼痛无作用。而纳布啡是阿片受体的激动-拮抗混合型镇痛药,主要对μ受体呈拮抗作用,对κ受体呈激动作用,κ受体激动剂在多种内脏痛模型中全身性注射后会产生强效镇痛,可用于治疗多种内脏痛,包括腹部手术镇痛、痛经、产痛以及应激性结肠综合征或消化不良等胃肠功能紊乱,尤其适用于妇产科患者的镇痛[14-15]。纳布啡镇痛强度与吗啡相当,可用于治疗和预防中度至重度疼痛,且成瘾性小,较吗啡有更高的安全性;同时心血管系统副作用少,呼吸抑制轻微,且有封顶效应;还可拮抗μ受体相关的不良反应,如恶心、呕吐、瘙痒等[16]。毕小宝等[17]研究发现,纳布啡比舒芬太尼更少发生呼吸抑制、呕吐、头晕等并发症。Chen等[18]在门诊无痛人工流产术的麻醉中使用纳布啡,与舒芬太尼比较,头晕发生率更低,觉醒时间与离开医院时间更短,进一步提示纳布啡比常用的舒芬太尼更适合日间手术。
综上所述,术前TAP阻滞进行超前镇痛,联合纳布啡更能完善术后镇痛,能让患者术中生命体征平稳,减少术中、术后阿片类镇痛药量,提前复苏、进食等,有利于日间妇科腹腔镜手术的快速康复。
[参考文献]
[1]鲍杨,贺广宝,张丽峰,等.日间手术麻醉安全性探讨[J].医学与哲学(B),2014,35(4):86-87.
[2]Markic D,Vujicic B,Ivanovski M,et al.Peritoneal dialysis catheter placement using an ultrasound guided transversus abdominis plane block[J].Blood Purif,2015,39(4):274-280.
[3]Anwar S,Brien B.The role of intraoperation interventions to minimize chronic postsurgical pain[J].Br J Pain,2017,11(4):186-191.
[4]El-Dawlatly AA,Turkistani A,Kettner SC.Ultrasound-guided transverses abdominisplane block:description of a new technique and comparison with conventional systemic analgesia during laparoscopic cholecystectomy[J].Br J Anaesth ,2009,102(6):763-767.
[5]Kagwa S,Hoeft MA,Firth PG,et al.Ultrasound guided transverses abdominis plane versus sham blocks after caesarean section in an Ugandan village hospital:a prospective,randomized,double-blinded,single-centre study[J].Lancet,2015, 385(S2):S36.
[6]周春莲,杨燕青,汪小丹.超声引导下腹横肌平面阻滞对于妇科腹腔镜手术患者预防性镇痛的效果[J].中国内镜杂志,2018,24(3):75-79.
[7]Ali HM,Shehata AH.Open appendectomy using ultrasound guided transverses abdomimis plane block:a case report[J].Anesth Pain Med,2017,7(2):e38118.
[8]Ma N,Duncan JK,Scarfe AJ.et al.Clinical safety and effectiveness of transversus abdominis plane (TAP) block in post-operative analgesia:a systematic review and meta-analysis[J].J Anesth,2017,31(3):432-452.
[9]牟俊英,赵博,袁泉,等.超声引导腹横肌平面阻滞对无张力疝修补术后患者疼痛及生存质量的影响[J].实用医学杂志,2018,34(15):2541-2543,2547.
[10]李煜,易艳萍,陈金海.腹横肌平面阻滞复合全身麻醉在日间腹腔镜子宫肌瘤剔除手术的应用[J].中国当代医药,2018,25(36):61-63.
[11]徐桂萍,潘阳阳,乔南南,等.腹横平面阻滞在老年高危患者腹肌沟疝修补术中的应用[J].临床麻醉学杂志,2018, 34(7):639-642.
[12]Mugita M,Kawahara R,Tamai Y,et al.Effectiveness of ultrasound-guided transversus abdominis plane block and rectus sheath block in pain control and recovery after gynecological transumbilical single-incision laparoscopic surgery[J].Clin Exp Obstet Gynecol,2014,41(6):627-632.
[13]Kim AJ,Yong RJ,Urman RD.The rRole of transversus abdominis plane blocks in ERAS pathways for open and laparoscopic colorectal surgery[J].J Laparoendosc Adv Surg Tech A,2017,27(9):909-914.
[14]French CA,Cong X,Chung KS.Labor epidural analgesia and breast-feeding:a systematic review[J].J Hum Lact,2016,32(3):507-520.
[15]鲍静影,杨云.纳布啡在妇产科麻醉中的应用发展[J].中国新药与临床杂志,2018,37(8):439-442.
[16]Zeng Z,Lu JH,Shu C,et al.A comparision of nalbuphine with morphine for analgesic effects and safety:meta-analysis of randomized controlled trials[J].Sci Rep,2015,5:10 927.
[17]畢小宝,王琼,张高龙,等.纳布啡与舒芬太尼用于宫腔镜手术的麻醉效果比较[J].实用医学杂志,2018,34(18):3085-3088.
[18]Chen L,Zhou Y,Cai Y,et al.The ED95 of Nalbuphine in outpatient-induced abortion compared to equivalent Sufentanil[J].Basic Clin Pharmacol Toxicol,2018,123(2):202-206.
(收稿日期:2019-03-11? 本文编辑:任秀兰)

