赵栋 吕华燕 刘晴晴 蓝志坚 徐军

[摘要] 目的 采用開胸前肺萎陷技术评价不同支气管封堵时间对胸腔镜手术肺萎陷效果的影响。 方法 选择2019年8~12月在我院行胸腔镜左肺楔形切除术的患者75例,采用随机数字表法将其分为三组,每组各25例。三组均采用开胸前肺萎陷技术,使用支气管封堵器行肺叶隔离。A组患者支气管封堵8 min后进胸,B组患者支气管封堵10 min后进胸,C组患者支气管封堵12 min后进胸。记录每组侧卧位即时(T0)和打开胸膜前(T1)的HR、SBP、DBP、SpO2、PaO2、PaCO2,并且各组到封堵时间点后即刻进胸,在胸腔镜直视下观察此刻的肺萎陷情况并评分。 结果 与A组比较,B组和C组患者的肺萎陷评分显著增加,差异有统计学意义(P<0.05);B组和C组之间的肺萎陷评分比较,差异无统计学意义(P>0.05)。三组患者T1时的PaO2较T0时显著下降(P<0.05);T1时三组患者PaO2组间比较,差异有统计学意义(统计值为F=5.193,P=0.008);C组患者T1时SpO2较T0时显著下降(P<0.05);T1时三组患者的SBP、DBP、HR比较,差异无统计学意义(P>0.05)。 结论 开胸前肺萎陷技术对促进开胸前肺萎陷有效,对血流动力学无明显影响。支气管封堵10 min既可达到良好的开胸前肺萎陷效果,又可保持良好的SpO2,适合作为胸腔镜进胸时机。
[关键词] 胸腔镜检查;纯氧;肺萎陷;吸收性肺不张
[中图分类号] R561? ? ? ? ? [文献标识码] B? ? ? ? ? [文章编号] 1673-9701(2020)32-0059-05
[Abstract] Objective To evaluate the impacts of efficacies of different bronchial occlusion time on pulmonary atrophy in thoracoscopic surgery by using technique of pulmonary atrophy before thoracotomy. Methods A total of 75 patients who underwent thoracoscopic wedge resection of left lung from August to December 2019 in our hospital were selected. They were divided into three groups according to the random number table method, 25 cases in each group. All the three groups were isolated by bronchial occlusive device to perform pulmonary lobe isolation, and the pulmonary atrophy technique before thoracotomy was adopted. Patients in group A were treated by thoracotomy after bronchial occlusion for 8 minutes. Patients in group B were treated by thoracotomy after bronchial occlusion for 10 minutes. Patients in group C were treated by thoracotomy after bronchial occlusion for 12 minutes. HR, SBP, DBP, SpO2, PaO2, PaCO2 were recorded immediately in lateral position(T0) and before pleura opening(T1) in each group, and the thoracotomy was performed immediately after each occlusion time point. Meanwhile, the pulmonary atrophy score was observed and evaluated under thoracoscopic vision. Results Compared with group A, the pulmonary atrophy scores of patients in group B and C were increased significantly(P<0.05). And there was no significant difference in pulmonary atrophy scores between group B and group C(P>0.05). PaO2 of the three groups of patients decreased significantly at T1 compared with T0(P<0.05). And at T1, the PaO2 values of the three groups of patients were significantly different(statistical values were F=5.193 and P=0.008). While SpO2 of patients in group C decreased significantly at T1 compared with T0(P<0.05). At T1, there were no significant differences in SBP, DBP and HR among the three groups of patients(P>0.05). Conclusion The technique of pulmonary atrophy before thoracotomy is effective in promoting pulmonary atrophy before thoracotomy and has no obvious impacts on hemodynamics. Bronchial occlusion for 10 minutes can not only achieve good effect of pulmonary atrophy before thoracotomy, but also maintain good SpO2, which is the suitable timing for thoracoscopic thoracotomy surgery.
[Key words] Thoracoscopy; Pure oxygen; Pulmonary atrophy; Resorption atelectasis
支气管封堵器(Bronchial blocker,BB)可应用于胸腔手术时的单肺通气(One-lung ventilation,OLV),与双腔支气管导管(Double lumen endobronchial tube,DLT)比较,具有插管、定位容易、心血管反应小、呼吸道损伤小的优点[1-3]。但BB的一大缺点是肺萎陷时间长[4-6],这是限制其在视频胸腔镜手术(Video-assisted thoracic surgery,VATS)中应用的一个原因。近年来随着BB肺萎陷技术的改进,肺萎陷的效率接近甚至超过双腔支气管导管[7-8]。Pandhi等[9]报道断开技术比自然塌陷更有助于加速BB的肺萎陷。El-Tahan[10]报道应用-30 cm H2O吸力在BB的吸引管口持续支气管吸引,肺萎陷所需的时间比断开方法明显缩短。即便如此,对于手术安全而言,更有意义的是能在胸膜打开之前完成肺萎陷,因为VATS进胸时间很短,对术侧肺萎陷和手术野的要求很高。依据本项目组的前期研究成果(实用新型专利号:ZL201820336679.5),开胸前肺萎陷技术被证实有效。为更深入地了解该技术的可行性和安全性,本项目组进行前瞻性随机对照研究,现报道如下。
1 资料与方法
1.1一般资料
选择2019年8~12月在我院行胸腔鏡左肺楔形切除术的患者75例,根据前期研究成果,采用随机数字表法将患者分为三组:A组(支气管封堵8 min)、B组(支气管封堵10 min)和C组(支气管封堵12 min),每组各25例。纳入标准:美国麻醉医师协会分级中,诊断为Ⅰ级、Ⅱ级,年龄30~79岁,体质量指数(BMI)<30 kg/m2。排除标准:预期的困难气管插管、严重的慢性阻塞性肺疾病史、胸膜和(或)间质性疾病史、胸腔放疗史及肺功能FEV1<50%预测值。本研究经我院医学伦理委员会批准,患者及家属签署知情同意书。本研究手术均为我院同一组外科医师完成,手术方式选择三孔胸腔镜。三组患者一般情况(性别、年龄、BMI)、术前血红蛋白、肺功能指标[用力肺活量占预计值百分比(FVCex%)、第1秒用力呼气容积占预计值百分比(FEV1%)、第1秒用力呼气容积占预计值百分比(FEV1/FVCex%)、弥散量占预计值百分比(TLCO%)]比较,差异无统计学意义(P>0.05)。见表1。
1.2 方法
患者入室后常规监测血压(Blood pressure,BP)、脉博血氧饱和度(Pulse oxygen saturation,SpO2)、心电图(ECG)、呼气末二氧化碳分压(PETCO2)。局麻下桡动脉穿刺并监测有创动脉压(Arterial blood pressure,ABP)。麻醉诱导采用咪唑安定0.05 mg/kg,舒芬太尼0.5~1.0 μg/kg,依托咪酯脂肪乳0.2 mg/kg,顺苯磺酸阿曲库铵0.2 mg/kg。肌肉松弛后,先后置入ID 8 mm的单腔气管导管和Coopdech支气管封堵器(杭州坦帕医疗科技有限公司),在距离隆突3 cm的位置放置封堵器球囊。三组患者均在纤维支气管镜下确认位置后,连接麻醉机行双肺通气,潮气量8~10 mL/kg,呼吸频率12 bpm,呼吸比(I∶E)1∶2,吸入氧浓度(Fraction of inspiration O2,FiO2)100%。术中用微量注射泵持续静脉输注丙泊酚3~5 mg/(kg·h)、瑞芬太尼0.1~0.3 μg/(kg·min),顺苯环酸阿曲库铵0.1 mg/kg间断注射维持麻醉,使脑电双频指数(Bispect ral index,BIS)值维持40~60。
三组患者双肺纯氧通气时间均不少于3 min,应用开胸前肺萎陷技术,即去氮通气后,在右侧卧位前即刻充气BB管气囊,行左支气管封堵,并行单肺通气,BB吸引管被故意堵塞。侧卧位之前封堵支气管是本技术中的一个重要环节,患者侧卧位后再次用纤维支气管镜确认气囊位置,在进胸前单肺通气期间,呼吸参数不变。A组患者支气管封堵到8 min时即刻打开观察孔并置入胸腔镜,B组患者支气管封堵10 min后进胸,C组患者支气管封堵12 min后进胸。手术团队需在各组相应封堵时间内完成消毒、铺巾、装镜套等进胸前准备工作。胸膜打开10 min后,调整呼吸机设置,下调FiO2和VT,以使峰值压力保持在25 cmH2O以下。
1.3 观察指标
(1)记录每组患者侧卧位即时(T0)和封堵到各时间点(T1)的HR、收缩压(SBP)、舒张压(DBP)和SpO2。(2)记录两个时间点动脉血气中的动脉血氧分压(Partial pressure of oxygen of arterial blood,PaO2)和PaCO2。(3)记录OLV开始至胸膜打开期间SpO2下降(SpO2<99%)和低氧血症(SpO2≤90%)发生情况。如在该过程中患者SpO2<90%,即表示缺氧,则改为双肺通气并终止试验。(4)肺萎陷的质量:封堵到各时间时嘱手术医师打开腔镜观察孔放置Troca,并在胸腔镜进胸后不同角度拍摄三张照片,术后由第三方同一位外科医师使用非参数性语言评价量表对肺萎陷进行评分:从0分(无肺萎陷)到10分(最大肺萎陷)[11]。
1.4 统计学方法
数据应用SPSS18.0统计学软件进行分析,符合正态分布的计量资料用(x±s)表示,采用t检验;不符合正态分布的计量资料用M(QL,QU)表示,采用秩和检验;计数资料用[n(%)]表示,采用χ2检验,P<0.05为差异有统计学意义。
2 结果
2.1 三组肺萎陷评分比较
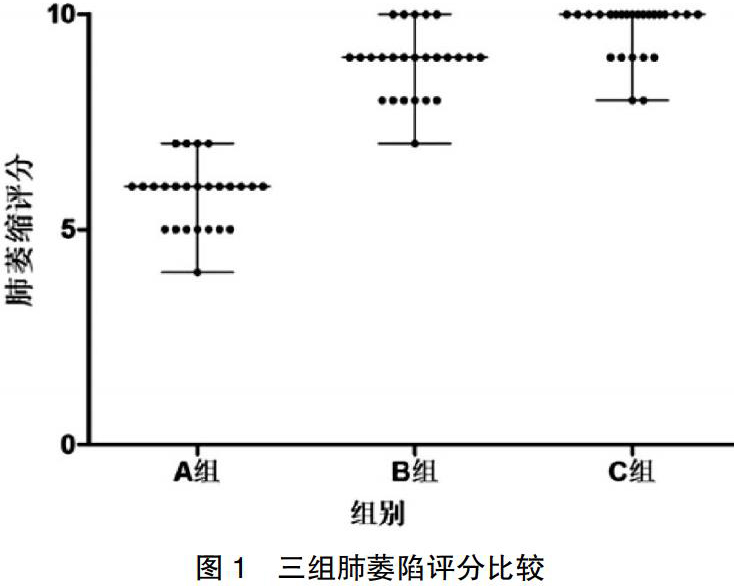
T1时三组的肺萎陷评分分别为A组6(4,7)分,B组9(8,10)分,C组10(8,10)分。与A组比较,B组和C组患者的肺萎陷评分显著增加,差异有统计学意义(P<0.05);B组和C组患者的肺萎陷评分比较,差异无统计学意义(P>0.05)。见图1。
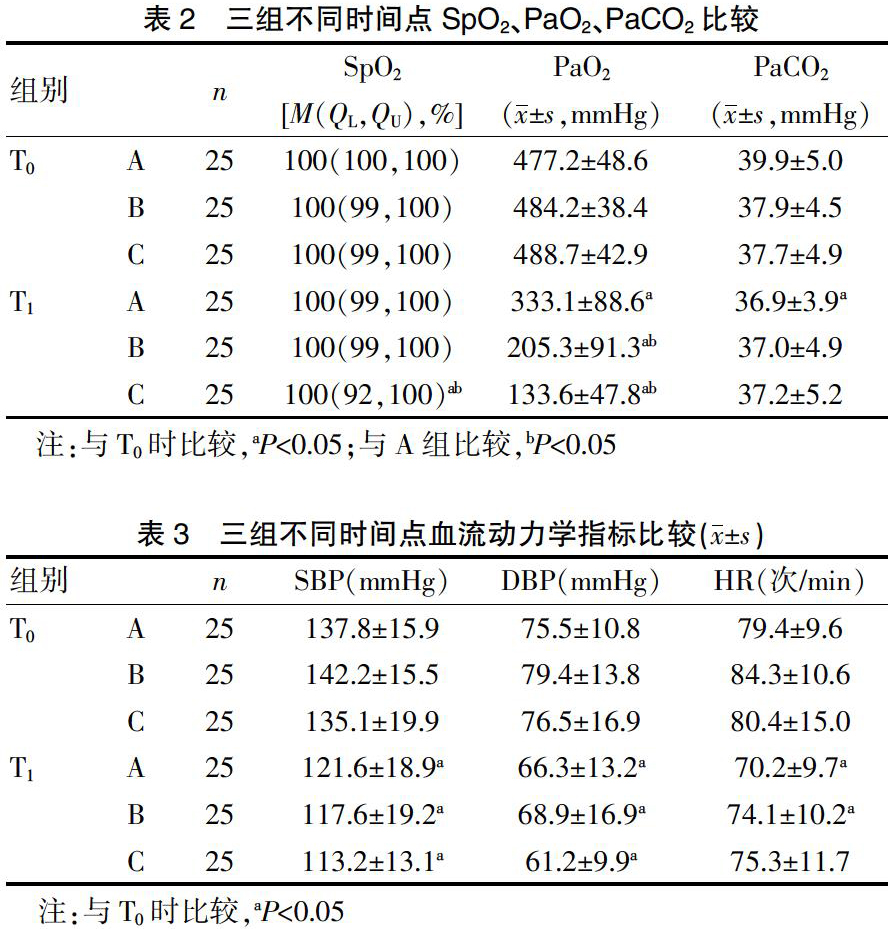
2.2 三组不同时间点SpO2、PaO2、PaCO2比较
A组和B组的SpO2在T1时和T0时比较,差异无统计学意义(P>0.05),C组的SpO2在T1时较T0时显著下降,差异有统计学意义(P<0.05);三组PaO2在T1时较T0时均显著下降(P<0.05),在T1时组间比较,差异有统计学意义(F=5.193,P=0.008)。见表2。
2.3三组不同时间点血流动力学指标比较。
T0及T1时三组患者的SBP、DBP、HR组间比较,差异无统计学意义(P>0.05);三组患者T1时的SBP、DBP较T0时显著下降,差异有统计学意义(P<0.05);A组和B组在T1时的HR较T0时显著下降,差异有统计学意义(P<0.05)。见表3。
2.4 三组T1进胸时肺萎陷效果比较
三组T1时胸腔镜进胸即刻所示肺萎陷效果(封三图5)。
3讨论
先前的一项研究显示[12],肺萎陷可分为两个阶段:胸膜一旦打开,此时肺萎陷主要依靠Ⅰ相肺萎陷,即肺固有弹性回缩力使肺部立即发生局部萎陷,但60 s后Ⅰ相肺萎陷停止[13],分析其原因与小气道闭合相关,即使采取气道吸引,也无法将肺泡内气体完全排出[14]。随后出现的是缓慢的Ⅱ相肺萎陷,这取决于持续的气体扩散和吸收性肺不张。因此,要改善肺萎陷的时效性,应试图提高Ⅱ相肺萎陷的速度。
开胸前肺萎陷技术是指在胸腔镜手术中,胸膜打开之前术侧肺即达到或接近完全萎缩效果的技術,是一种肺的主动萎缩,其依据主要是Ⅱ相肺萎陷,即残余肺泡气的持续吸收或吸收性肺不张。其中残留气体的再吸收速率与溶解度呈正比,氧气有溶解度大和能与Hb结合的特性,存在肺泡内可快速被机体所吸收[15]。此时FiO2增加,患侧肺残存气体的吸收率显著加快,双肺通气期间去除肺内氮气是改善肺萎陷的有效策略[16-17]。Pfitzner等[18]的动物试验显示,在胸腔镜手术期间,使用纯氧或氧气/一氧化二氮混合物进行机械肺通气,会增加从非通气侧肺中吸收气体的速度,从而加快其吸收性肺不张。本研究选择在支气管封堵之前双肺纯氧通气3 min以上,同时BB排气管处于封闭状态,这是本技术的一个重要环节,因为封闭可以使术侧肺形成弥散呼吸状态,即无呼吸运动,只有摄氧而不能排出二氧化碳的呼吸状态[19]。本技术中的另一个重要环节是侧卧位之前封堵支气管,因为在前期研究中发现,侧卧位之后实施支气管封堵,并不都能产生良好的肺萎陷效果,可能的原因是侧卧位下由于重力作用,封堵侧肺循环量因流向了通气侧肺而减少,导致肺泡内氧气不能快速地弥散至肺循环中,影响肺萎陷效果。
本研究结果显示,与A组比较,B组和C组患者的肺萎陷评分显著增加,差异有统计学意义(P<0.05);B组和C组之间的肺萎陷评分比较,差异无统计学意义(P>0.05),均达到或接近完全萎缩。说明开胸前肺萎陷技术是有效的,结果显示术侧支气管封堵10 min及以上,术侧肺便可以达到优良的萎缩效果。见图1。
研究一种肺萎陷方法时,安全性非常重要,是否发生低氧血症是一项重要的安全指标。本研究结果显示,在T1时B组和C组的PaO2较A组显著下降,差异有统计学意义(P<0.05)。原因可能是应用开胸前肺萎陷技术,随着封堵时间的延长,肺泡逐渐萎缩,肺内压逐渐下降,并由正压转为负压,导致患侧肺血流下降不明显甚至增加,使术侧肺组织通气/血流比例失调,造成静脉血掺杂,肺内分流增大,导致PaO2的下降及Qs/Qt的明显增加[20];同时,肺血流增加进一步促进肺泡内氧气的吸收,加速肺泡萎缩。PaO2的下降会使SpO2下降,本研究结果显示,T1时B组的SpO2和A组无显著差异,但C组较A组显著下降。统计数据显示C组中有20%(5例)的患者出现SpO2下降,但无一例出现低氧血症,并且在胸膜打开后SpO2迅速恢复。说明封堵10 min较封堵12 min更能保持良好的SpO2。
本研究结果显示,T1时三组患者的HR、SBP和DBP比较,差异无统计学意义(P>0.05),说明开胸前肺萎陷技术并未影响到血流动力学的稳定。原因可能是患侧肺萎陷产生的胸腔负压和纵膈重力相互抵消,并不会造成纵膈的明显偏移而使血管扭曲;另外,胸腔负压也会增加心脏前负荷,避免血压下降。
但本研究过程中仍有一些局限。首先,本研究设定从OLV到胸膜打开的时间为8~12 min,在此期间内完成消毒铺巾等进胸前准备工作,需要手术医生积极配合,本研究中消毒铺巾的医生不参与体位放置以便提前洗手。其次,在胸膜开放前的OLV期间出现一定比例的SpO2下降,如果OLV时间延长有可能会增加该比例。再者,在开胸前肺萎陷不理想的情况下,胸腔镜观察孔打孔时电刀或Troca可能会损伤肺组织,对于该问题本研究组将会通过监测气道压评估肺萎陷程度,以解决上述肺损伤问题。
综上所述,应用开胸前肺萎陷技术可以达到良好的开胸前肺萎陷效果,对血流动力学无明显影响;支气管封堵10 min和12 min均可达到良好的肺萎陷效果,但封堵10 min更能保持良好的SpO2,适合作为胸腔镜进胸时机。
[参考消息]
[1] Alison FB,Lisa ME.Successful combination of neuraxial and regional anesthesia in a child with advanced spinal muscular atrophy type 1 receiving maintenance nusinersen therapy:A case report[J].A & A Practice,2020,14(6):e01206.
[2] Zheng M,Niu Z,Chen P,et al.Effects of bronchial blockers on one-lung ventilation in general anesthesia:A randomized controlled trail[J].Medicine(Baltimore),2019,98(41):e17387.
[3] Bharat S,Virendra S.Diaphragmatic dysfunction in chronic obstructive pulmonary disease[J].Lung India,2019,36(4):285-287.
[4] Chou,SH,Lin GT,Shen PC,et al.The effect of scoliosis surgery on pulmonary function in spinal muscular atrophy type Ⅱ patients[J].European Spine Journal:Official Publication of the European Spine Society,the European Spinal Deformity Society,and the European Section of the Cervical Spine Research Society,2017,26(6):1721-1731.
[5] Emmanuel V,Armand MD.Bedside ultrasound for weaning from mechanical ventilation[J].Anesthesiology,2020, 132(5):947-948.
[6] Ehsanian R,Klein C,Mohole J,et al.A novel pharyngeal clearance maneuver for initial tracheostomy tube cuff deflation in high cervical tetraplegia[J].American Journal of Physical Medicine and Rehabilitation,2019,98(9):835-838.
[7] Meyer JE,Finnberg NK,Chen L,et al.Tissue TGF-beta expression following conventional radiotherapy and pulsed low-dose-rate radiation[J].Cell Cycle,2017,16(12):1171-1174.
[8] Zhang Q,Wang MH,Li WQ,et al.Left lung neoplasms and bilateral pleural effusion combined elevated carcinoembryonic antigen in pleural effusion with negative result of thoracoscopy pleural biopsy misdiagnosed as lung carcinoma ultimately confirmed pulmonary sarcomatoid carcinoma by CT-guided percutaneous lung biopsy:A case report and literature review[J].Clinical Laboratory,2019,65(8):1547-1550.
[9] Pandhi N,Kajal N,Rana S.CR-21 utility of thoracoscopy in diagnosis of lung tumour in pleural effusion[J].Journal of Thoracic Oncology:Official Publication of the International Association for the Study of Lung Cancer,2018,13(10):S1036.
[10] El-Tahan MR.A comparison of the disconnection technique with continuous bronchial suction for lung deflation when using the arndt endobronchial blocker during video-assisted thoracoscopy:A randomised trial[J].Eur J Anaesthesiol,2015,32:411-417.
[11] Magdy O,Ahmad A,Nashwa E,et al.The role of medical thoracoscopic lung biopsy in diagnosis of diffuse parenchymal lung diseases[J].Egyptian Journal of Bronchology,2019, 13(2):155-161.
[12] Pfitzner J,Peacock MJ,Harris RJ.Speed of collapse of the non-ventilated lung during single-lung ventilation for thoracoscopic surgery:The effect of transient increases in pleural pressure on the venting of gas from the non-ventilated lung[J].Anesthesia,2001,56:940-946.
[13] Ip H,Ahmed S,Noorzad F,et al.Non-expandable lung in malignant pleural effusions at medical thoracoscopy[J].Thorax:The Journal of the British Thoracic Society,2018,73(4):A259.
[14] Myeong GC,Sojung P,Dong KO,et al.Effect of medical thoracoscopy-guided intrapleural docetaxel therapy to manage malignant pleural effusion in patients with non-small cell lung cancer:A pilot study[J].Thoracic Cancer,2019,10(10):1885-1892.
[15] Ochiai R.What should we know about respiratory physiology for the optimal anesthesia management?[J].Masui,2016,65(5):442-451.
[16] Li XX,Xing GW,W JY,et al.Predictors of survival in non-small cell lung cancer patients with pleural effusion undergoing thoracoscopy[J].Thoracic Cancer,2019,10(6):1412-1418.
[17] Pfitzner J,Peacock MJ,Daniels BW.Ambient pressure oxygen reservoir apparatus for use during one-lung anaesthesia[J].Anaesthesia,1999,54:454-458.
[18] Pfitzner J,Peacock MJ,Pfitzner L.Speed of collapse of the non-ventilated lung during one-lung anaesthesia:The effects of the use of nitrous oxide in sheep[J].Anaesthesia,2001,56(10):933-939.
[19] 莊心良,曾因明,陈伯銮.现代麻醉学[M].3版.北京:人民卫生出版社,2003:61.
[20] Verhage RJ,Boone J,Rijkers GT,et a1.Reduced local immune response with continuous positive airway pressure during one-lung ventilation for oesophagectomy[J].Br J Anaesth,2014,112(5):920-928.
(收稿日期:2020-05-18)
- 中职学校如何开展心理健康教育
- 融合翻转课堂与传统课堂的中职平面设计教学设计
- 农村中小学教师“研训一体”模式建构探究
- 指向生存智慧的高中网络德育实践研究
- 浅谈农村中学校园欺凌现状及防治策略
- 农村初中实施分层走班教学的实践和思考
- 踏浪潮头寻技巧 引领花朵绽新颜
- 打造美育特色 提升学校品位
- 聚焦学生主体精神 创新学校育人渠道
- 浅析数学自主探究课堂的有效提问
- 试析初中数学课堂启发式教学
- 高中数学学历案编制研究及案例
- 关于初中数学课堂导入法的若干思考
- 山区初中数学课堂教学模式探析
- 数学实验在高中数学探究教学中的应用
- 渗透语文课堂 传承民族文化
- 信息化时代下初中计算机课程教学问题分析及对策
- 浅谈如何打造中小学信息技术高效课堂
- 基于美育理论的初中信息技术课堂教学模式探究
- 提高信息技术实践课教学效率之方法浅析
- 高中信息技术活动式课堂构建与实践
- 信息技术动画课堂“问题化教学”实践
- 解读《项脊轩志》里的空间情境
- 《卖油翁》的深层意蕴探析
- 联结生活,让语文教学更有效
- be in power
- be in prison/jail
- cornstarch
- cornstarches
- corny
- corollaries
- corollary
- coronaries
- coronary
- coronary²
- coronary¹
- coronation
- coronations
- coroner
- coroners
- coronership
- coronerships
- corp.
- corp
- corporal
- corporalcies
- corporalcy, corporalship
- corporalcy's
- corporalities'
- corporality's
- 老中医把脉
- 老中青
- 老中青三结合
- 老串
- 老主人
- 老主意
- 老乃
- 老么
- 老之将至
- 老乌龟
- 老九
- 老九的弟弟——老实(十)
- 老也出不了声
- 老乡
- 老乡找老乡,一切好商量
- 老乡见老乡,两眼泪汪汪
- 老书
- 老乱
- 老了
- 老了的千里马还不如一条狗
- 老了脸皮,饱了肚皮
- 老了还学吹鼓手
- 老二
- 老二哥
- 老于世故