何禾 杨沿浪
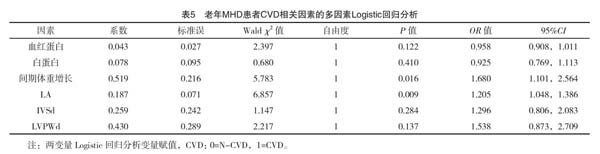

【摘要】 目的:了解导致老年維持性血液透析(maintain hemodialysis,MHD)患者发生心血管疾病的影响因素。方法:选择2016年1月-2019年11月在皖南医学院第二附属医院进行维持性血液透析治疗的老年慢性肾衰竭患者74例。按照是否发生心血管疾病(cardiovascular disease,CVD)分为CVD组(n=36),N-CVD组(n=38)。收集一般病史资料、实验室数据、彩色超声心动图指标。采用单因素、多因素Logistic回归分析方法进行统计学分析。结果:两组透析方式、间期体重增长、血红蛋白、白蛋白、左房内径、左室射血分数、舒张期室间隔厚度、舒张期左室后壁厚度比较差异有统计学意义(P<0.05);在单因素Logistic分析结果中,血红蛋白、白蛋白是发生CVD的保护性因素,而间期体重增加、左房内径、舒张期室间隔、舒张期左室后壁厚度是危险因素(P<0.05);多因素Logistic分析结果中,左房内径、间期体重增加是老年MHD患者并发CVD的独立危险因素(P<0.05)。结论:左房内径增大、间期体重增加对老年MHD患者发生CVD具有重要的影响。
【关键词】 老年患者 维持性血液透析治疗 心血管疾病 危险因素
doi:10.14033/j.cnki.cfmr.2020.19.017 文献标识码 B 文章编号 1674-6805(2020)19-00-04
The Related Factors of Cardiovascular Disease in Elderly Patients Receiving Long-term Hemodialysis/HE He, YANG Yanlang. //Chinese and Foreign Medical Research, 2020, 18(19): -46
[Abstract] Objective: To investigate the related factors of cardiovascular disease (CVD) in elderly patients receiving long-term hemodialysis (HD). Method: A total of 74 elderly patients who received HD therapy in the Second Affiliated Hospital of Wannan Medical College from January 2016 to November 2019 were selected. The patients were divided into two groups by cardiovascular disease (CVD): CVD group (n=36) and N-CVD group (n=38). General medical history, laboratory data and color echocardiography were collected. Single factor and multi factor Logistic regression analysis was used for statistical analysis. Result: There were significant differences in dialysismode, IDWG, hemoglobin, albumin, LA, IVSd, LVPWd, LVEF between CVD group and N-CVD group (P<0.05). The univariate Logistic regression analysis showed that hemoglobin and albumin were protective factors for CVD, while weight gain, left atrial diameter, diastolic interventricular septum and diastolic posterior wall thickness were risk factors (P<0.05). Multivariate Logistic regression analysis revealed that LA, IDWG were independent risk factor of CVD in HD patients (P<0.05). Conclusion: LA, IDWG are independent risk factor of CVD in patients receiving long-term hemodialysis.
[Key words] Elderly patients Long-term hemodialysis Cardiovascular disease Risk factor
First-authors address: The First Affiliated Hospital of Wannan Medical College, Wuhu 241000, China
人口老龄化问题日趋严重,在血液净化治疗领域,老年维持性血液透析(maintain hemodialysis,MHD)患者数量也在持续上升[1]。其中心血管疾病是MHD患者的首要死亡原因[2]。老年MHD患者常常患有高血压、糖尿病等基础疾病,动脉硬化程度较为严重,更易发生心血管疾病[3]。对此本研究预通过收集老年维持性血液透析患者的一般临床资料、实验室数据及心脏结构变化来探讨老年MHD患者发生心血管疾病(cardiovascular disease,CVD)的相关影响因素,现报告如下。
慢性容量超负荷是MHD患者的常见并发症,也是老年MHD患者常见情况。由于缺乏准确的估算方式,维持性血液透析治疗患者的细胞外液容量往往是过高的[11]。长期的慢性容量超负荷激活了肾素血管紧张素醛固酮系统,引起交感神经兴奋,导致血管收缩、心脏后负荷增加;回心血量增加后加重心脏前负荷,导致心脏结构改变,诱发心力衰竭[12]。在本次研究中CVD组的透析间期体重增加情况较大,两组间差异有统计学意义(P>0.05)。并且在多因素二元Logistic回归中,透析间期体重增加是老年MHD患者发生CVD的独立危险因素(OR=1.680,95%CI:1.101,2.564,P=0.016)。这些情况可导致老年MHD患者慢性容量负荷过重持续不缓解诱发CVD发生。
低血红蛋白是导致CVD发生的常见原因[13]。老年患者常常存在铁摄入不足、隐匿性的出血的情况,加重肾性贫血。在本次的研究结果中,低血红蛋白为老年MHD患者发生CVD的影响因素。蛋白能量消耗亦是导致MHD患者发生CVD的危险因素[14]。在Komatsu等[15]的研究中,发生低白蛋白的MHD患者血症常常伴随左心功能障碍,并且低白蛋白血症与高心血管疾病发病率及病死率有关。老年MHD患者由于纳差、消化吸收功能差,蛋白能量消耗更为严重。在本次研究中CVD组的白蛋白水平明显低于N-CVD组,单因素回归分析中白蛋白水平亦是老年MHD患者发生CVD的保护性因素(OR=0.925,P=0.410)。
在透析方式选择上,由于老年患者血流动力学不稳定,以及经济上的原因,常常选择低通量透析器进行常规血液透析治疗。这种选择往往不利于中分子毒素的清除,如微球蛋白、硫酸吲哚酚、同型半胱氨酸等均有强的氧化应激作用。上述物质的长期蓄积可促进炎症介质释放、加强单核细胞趋化、损伤内皮细胞[16]。这种持续的炎症反应状态诱发CVD发生[17-18]。在本次研究中,选择高通量透析的老年MHD的CVD发生率明显低于N-CVD组,差异有统计学意义(P=0.020)。高通量透析由于其对中分子毒素的清除有效可以较好地控制血压、条件脂糖代谢、保护血管内皮细胞,从而改善心血管病死率[19]。因此,在條件允许的情况下建议老年MHD患者可较早的进行高通量透析治疗。
老年MHD患者中,低血红蛋白、左房增大、低蛋白血症、间期体重增加是CVD的影响因素,其中左房增大、间期体重增加是诱发CVD的独立危险因素。因此老年MHD患者控制间期体重增加,改善低蛋白血症、纠正贫血、选择高通量透析治疗可能减少CVD的发生。
参考文献
[1] Zhang L,Zhao M H,Zuo L,et al.China Kidney Disease Network(CK-NET)2015 Annual Data Report[J].Kidney Int Suppl(2011),2019,9(1):e1-e81.
[2]孙明继,赵新菊,唐盛,等.维持性血液透析死亡患者相关信息及贫血治疗情况的多中心回顾性分析[J].中国血液净化,2019,9(18):618-621.
[3] Ahmadmehrabi S,Tang W H W.Hemodialysis-induced cardiovascular disease[J].Seminars in Dialysis,2018,31(3):258-267.
[4] Navaneethan S D,Francis G S.Cardiovascular impact in patients undergoing maintenance hemodialysis: Clinical management considerations[J].International Journal of Cardiology,2017,232:12-23.
[5] Gregg L P,Carmody T,Le D,et al.A Systematic Review and Meta-Analysis of Depression and Protein-Energy Wasting in Kidney Disease[J].Kidney International Reports,2020,5(3):332-342.
[6]毛永辉,王海涛,陈献广.维持性血液透析患者的心脏结构改变及预后分析[J].中国血液净化,2013,12(9):465-469.
[7] Ishigami J,Iimori S,Kuwahara M,et al.Diagnostic value of B-type natriuretic peptide for estimating left atrial size and its usefulness for predicting all-cause mortality and cardiovascular events among chronic haemodialysis patients[J].Nephrology,2014,19(12):777-783.
[8] Omae K,Ogawa T,Yoshikawa M,et al.Left atrial dilatation and ST-T changes predict cardiovascular outcome in chronic hemodialysis patients[J].Heart Vessels,2012,27:610-617.
[9] Malik J,Lachmanova J,Kudlicka J,et al.Left Atrial Dysfunction in End-Stage Renal Disease Patients Treated by Hemodialysis[J].Nephron,2016,133(3):169-174.
[10]陈胜男,申燕.慢性肾脏病的心血管并发症研究进展[J].中国病理生理杂志,2019,35(8):1532-1536.
[11] Yilmaz Z,Yildirim Y,Aydin F Y,et al.Relationship between fluid status as assessed by bioimpedance analysis and NT-pro BNP,blood pressure and left ventricular mass index in hemodialysis patients[J].Clin Ter,2014,165(1):52-58.
[12]牛世慧,劉莉,王珣.血清Cys-C和NT-proBNP对维持性血液透析患者心血管事件发生的影响[J].贵州医科大学学报,2020,45(3):363-367.
[13]赵新菊.慢性肾脏病贫血与左心室肥厚[J].中国血液净化,2018,17(7):438-441.
[14] Afsar B,Agca E,Turk S.Comparison of erythropoietin resistance in hemodialysis patients using calcitriol,cinacalcet,or paricalcitol[J].J Clin Pharmacol,2015,55(11):1280-1285.
[15] Komatsu M,Okazaki M,Tsuchiya K,et al.A low serum albumin level predicts cardiovascular events in hemodialysis patients with preserved left ventricular ejection fraction[J].Int J Cli Med,2015,6(2):85-89.
[16] Speer T,Schunk S J,Fliser D.Chronic kidney disease-a cardiovascular high-risk constellation[J].Der Internist,2020,61(4):340-348.
[17]姚英,章友康.β2微球蛋白与透析相关淀粉样变[J].中华肾病研究电子杂志,2019,8(3):128-131.
[18]刘芳婕,徐天华,姚丽.维持性血液透析患者中血清同型半胱氨酸与心血管疾病相关性研究[J].中国实用内科杂志,2018,38(6):559-561.
[19]血液净化模式选择专家共识[J].中国血液净化,2019,18(7):442-472.
(收稿日期:2020-04-24) (本文编辑:郎序莹)
- “儒如五谷”视域下的“独尊儒术”
- 论信息文明建设的中国化实践
- 结构—关系—文化:新中国70年县域治理场域要素变迁图谱
- 新中国70年党政关系的演进历程与基本经验
- 消解与重构:农村“厕所革命”的体制性障碍与制度化策略
- 环境、组织、主体:地方政府官员创新的三重动力机制分析
- 2019年总目录
- 宁波外来农民工社会融合度测评
- “一带一路”沿线的恐怖主义活动新态势解析
- 开放发展 合作共赢
- “一带一路”建设专题研究
- 对我国信用体系建设的政策建议
- 行政行为的表达方式研究
- “隐身党员”社区参与研究
- 以系统思维新理念引领基层党组织整体功能的强化
- 从“选举民主”到“协商民主”:英国工党的改革经验与启示
- 政治动员议题的建构、实施及效果评析
- 时代主题转换下中国发展道路的新探索
- 从“身份”到“契约”:当代中国农民公民身份的缺失与重构
- 中国是中华民族共同体标识的法制探讨
- 21世纪中国外交的国际发展伦理抉择
- 参加首届世界马克思主义大会琐记
- 新形势条件下中越经贸合作:对接与发展
- 中越关系:2014—2015年V字形发展
- 中越关系的困境与重构:一个方法论的思考
- pleaders
- pleadingly
- plead not guilty
- pleads
- pleas
- pleasable
- pleasant
- pleasanter
- pleasantest
- pleasantly
- pleasantness
- pleasantnesses
- pleasantries
- please
- please accept my apologies
- please be seated
- pleased
- pleased/good/nice to meet you
- pleasedly
- pleasedness
- pleasednesses
- pleased with yourself
- pleasely
- pleaser
- pleasers
- r2022090420002902
- r2022090420002903
- r2022090420002904
- r2022090420002906
- r2022090420002907
- r2022090420002908
- r2022090420002909
- r2022090420002910
- r2022090420002912
- r2022090420002913
- r2022090420002914
- r2022090420002915
- r2022090420002916
- r2022090420002918
- r2022090420002919
- r2022090420002920
- r2022090420002922
- r2022090420002923
- r2022090420002924
- r2022090420002926
- r2022090420002928
- r2022090420002929
- r2022090420002931
- r2022090420002932
- r2022090420002933